With the ability to capture detailed images of blood vessels in seconds, this breakthrough technology promises to revolutionize diagnostics in fields like rheumatology, oncology, and cardiovascular medicine.
Study: A fast all-optical 3D photoacoustic scanner for clinical vascular imaging
In a recent study published in the journal Nature Biomedical Engineering, researchers developed a three-dimensional (3D) photoacoustic tomography (PAT) scanner for rapid vascular imaging.
Visualizing the microvasculature to sub-centimeter depths is necessary for effective clinical management of vascular abnormalities. Optical imaging techniques are promising in visualizing vascular flow, anatomy, and oxygenation. Nevertheless, optical scattering by tissue limits spatial resolution or penetration depth. While ultrasound imaging can address the resolution/depth limitations, it presents other challenges.
As such, photoacoustic imaging is an alternative that can overcome the limitations of ultrasound and optical imaging. In PAT, a pulsed laser beam illuminates the tissue; optical absorption by hemoglobin generates impulsive heating and, subsequently, broadband ultrasound waves. An image can be reconstructed by detecting these waves at the skin’s surface.
PAT overcomes range-resolution concerns since ultrasound waves are scattered less than photons in the tissue. Notwithstanding, PAT implementation presents instrumentation-related challenges. Conventional piezoelectric ultrasound detectors are commonly used in PAT scanners but have poor sensitivity for sub-100 µm element sizes and insufficient broadband frequency response.
The study and findings
In the present study, researchers built a fast, all-optical PAT scanner for clinical vascular imaging. The custom-built scanner comprised an optical parametric oscillator (OPO) and a Fabry-Perot (FP) ultrasound sensor. The OPO emits nanosecond laser pulses (700 to 900 nm) delivered via an optical fiber. Light from the fiber’s distal end produces a large beam incident on the head of the FP ultrasound sensor. The acoustically sensitive element is an FP interferometer (FPI).
After passing through the sensor, the beam flood-illuminates the tissue beneath, generating broadband ultrasound waves that propagate to the FPI. The interference between light reflected from two FPI mirrors modulates reflected optical power, which is read by scanning an array of ≤ 64 focused laser beams over the sensor’s surface. Two strategies were implemented to reduce image acquisition times.
First, the A-line acquisition rate was increased by parallelizing sensor readout and using high-pulse repetition frequency (PRF) excitation lasers. The second strategy involved compressed sensing, allowing for subsampling of the acoustic detection aperture, which reduced the number of A-lines needed for image construction. The scanner acquired 3D in vivo vascular images of healthy adults.
Images were reconstructed within a second using the k-space method from 34,560 A-lines; the A-line rate was 6,400 seconds (s), and the total scan duration was 5.4s. Overall, the scanner provided detailed images of the microvasculature to depths up to 15 mm; the images were comparable to or better in quality than previous FP scanners. Images acquired at 100 hertz (Hz) and 200 Hz PRFs at A-line rates of 6,400/s and 12,800/s reduced acquisition times to 3.2s and 1.6s, respectively.
Further, at 1 kHz, the A-line rate increased to 64,000/s, and the total scan time was 0.3s. Image quality was not excessively compromised. To demonstrate clinical utility, exploratory case studies were undertaken on patients with suspected vascular changes related to rheumatoid arthritis, peripheral vascular disease (PVD), and skin inflammation.
Images of the feet of patients at risk of small-vessel PVD were acquired. The patient’s right foot microcirculation was normal, but the left foot showed symptoms of impaired perfusion. Images showed vessel tortuosity in the left foot, which has been linked to PVD-associated microvasculopathy.
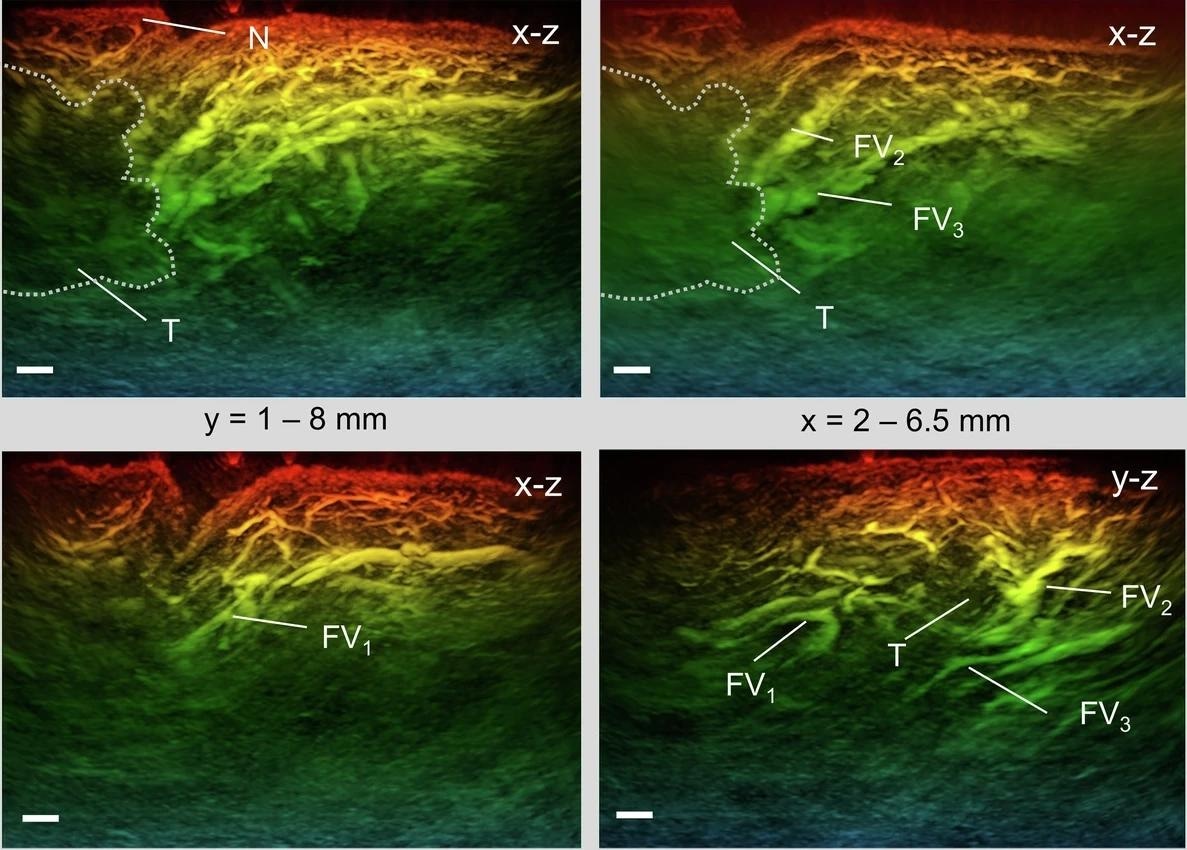
Next, the skin around a raised papule after an insect bite was imaged several times over seven days. On day 1, images revealed a dense, chaotic microvasculature extending from the epidermis to the hypodermis in the papule region. The number of vessels gradually diminished over time. Finally, the team scanned images of the interphalangeal joints of a rheumatoid arthritis patient.
The affected right-hand joint in the tendon region showed higher contrast than in the unaffected left-hand joint. Further, they scanned the joints of patients with increased disease severity and five healthy controls. Results showed significant differences between patients with active disease and controls, suggesting inflammation-induced neoangiogenesis could be detected.
Conclusions
Taken together, the researchers developed a high-resolution FP ultrasound sensor-based photoacoustic scanner and evaluated its potential as a clinical imaging tool. While early-generation FP scanners provide high-quality images, they require long scan times. This limitation was overcome through parallelized readouts, high-PRF excitation lasers, and compressed sensing. High-quality images can be acquired within seconds without compromising quality. Rapid, all-optical PAT could be useful in rheumatology, oncology, cardiovascular medicine, and dermatology.