In this interview from SfN 2024, Professor Nancy Ip, President of The Hong Kong University of Science and Technology, shares insights into her pioneering neuroscience research. She discusses her journey, breakthroughs in neurotrophic factors, and innovative approaches to Alzheimer’s disease treatment.
Professor Ip highlights immune modulation, brain signaling pathways, and the potential of traditional Chinese medicine in combating neurodegeneration. She also reflects on how new technologies and precision medicine are shaping the future of Alzheimer’s research and the importance of lifelong brain health.
To start, could you introduce yourself and share what drew you to neuroscience? How did your early research on neurotrophic factors shape your approach to studying brain development and neurodegenerative diseases?
I am Nancy Ip, the Morningside Professor of Life Science and President of The Hong Kong University of Science and Technology.
My interest in neuroscience began during graduate school. After earning my bachelor’s degree from Simmons College in Boston, I entered graduate school at Harvard Medical School, where I joined a neuroscience lab, drawn to the complexity and mystery of the brain. At that time, we knew very little about this highly intricate organ, and I was especially eager to explore how neurons communicate.
My thesis work identified a novel communication mechanism involving peptides such as VIP and secretin, a significant finding as the only known neurotransmitters in the mammalian system were small molecules like acetylcholine. I found that these peptides were utilized depending on the pattern of stimulation, and as a result of this novel discovery, I was the first author of several high-profile papers.
After completing my Ph.D., I did a postdoc, then took a year off before working at Lifecodes, a biotech company. While I enjoyed the work, I missed neuroscience research and realized that was where my true passion lay. So, when the chance arose to join Regeneron, a promising young startup focused on neurodegenerative diseases, I took it. At Regeneron, I worked on neurotrophic factors and contributed to the discovery of two neurotrophins (Neurotrophin-3 and Neurotrophin-4) as well as CNTF (ciliary neurotrophic factor). Our work advanced the field of neurotrophic factors, showcasing their role in neural development and plasticity. Regeneron’s contributions have had a lasting impact on neuroscience.
In 1993, I returned to Hong Kong and joined the Hong Kong University of Science and Technology (HKUST), marking the start of my academic career.
My initial academic research aimed to understand how neurotrophic factors and receptor signaling regulate synapses—the junctions where neurons communicate. Later, I shifted focus to the mechanisms underlying synaptic plasticity, which is fundamental to learning and memory. Our team made significant strides in these areas, paving the way to study Alzheimer’s disease (AD), a condition marked by memory loss. Since synapse loss is a key feature of AD, I became interested in investigating how dysregulation of neurotrophic factors contributes to synapse loss and impaired synaptic function in AD, which led to deeper, multi-level studies of the disease.
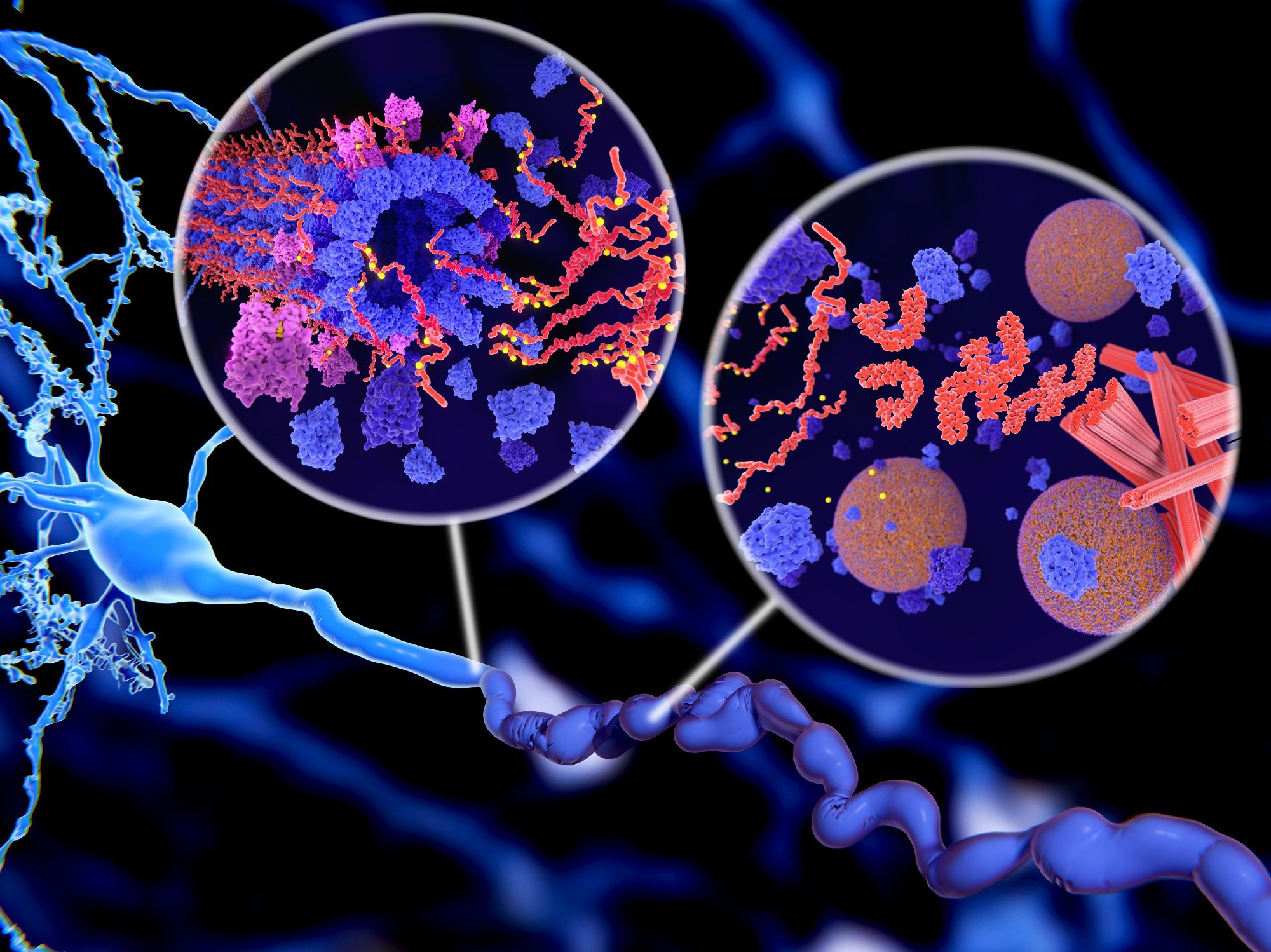 Image Credit: Juan Gaertner/Shutterstock.com
Image Credit: Juan Gaertner/Shutterstock.com
Your research on the immune system’s role in Alzheimer’s disease has been groundbreaking. How do you think these insights could transform the way we approach treating this condition?
Uncovering the role of the immune system in AD pathology has significantly enhanced our understanding of AD pathogenesis. Genetic evidence showing the association of immune system with AD further supports the roles of the impaired immune system in the pathogenesis of AD.
With better understanding of the molecular and cellular biology underlying immune system dysfunction, we are able to identify new molecular targets and develop novel disease-modifying treatment approaches. This knowledge can also help us better understand the anticipated outcomes from modulating the corresponding expression/activity of potential targets in model mice of AD.
Furthermore, genetics and biomarker studies are enabling us to predict and reveal the impaired immune system in AD. This information can be used to stratify patients with impaired immune functions. Thus, targeting the impaired immune system in AD could be used as a precision medicine approach.
How might your discoveries about brain signaling pathways lead to new therapies that improve cognitive function for patients with Alzheimer’s?
Our work on brain signaling pathways has identified new molecular targets and its associated biology as well as unveiled new therapeutic approaches.
For example, in our work on the cytokine IL-33, we found that activation of the signaling pathway, by administering IL-33 to AD model mice, decreases amyloid beta (Aβ) pathology and alleviates memory impairment in the mice.
This exciting discovery highlighted immune modulation as a potential AD treatment and IL-33 as a potential drug target, leading to the development of IL-33 modulators as potential therapeutics. Our subsequent studies revealed that IL-33 reduces Aβ pathology by mobilizing microglia, a major immune cell type in the brain, towards toxic Aβ to engulf and clear them.
Our study of the IL33/ST2 pathway also led to the discovery of a novel treatment approach. In this study, human data analysis revealed that blood levels of soluble ST2 (sST2), a decoy receptor of IL-33/ST2, increases in AD patients, while mouse model analysis revealed the action of sST2 on regulating molecular phenotypes and the functions of microglia. These insights highlighted sST2 as a promising drug target for AD, leading to the development of novel sST2 modulators as potential therapeutics.
The link between aging and the immune system is a key focus of your work. How do you think better understanding this connection could improve quality of life as people age?
A better understanding of this connection, particularly how the immune system changes with increasing age, will provide important insights on how to manage age-related diseases as well as promote healthy aging.
Aging is the strongest risk factor of AD. As Alzheimer’s researchers, it is important for us to understand the changes in specific immune biomarkers as individuals age and determine whether any of them serve as pathological factors or contribute to the pathogenesis of AD. Clearer understanding of how these biomarkers contribute to disease will help identify promising targets for drug development.
Knowledge of how the immune system changes with age can also help in developing preventive measures. This includes lifestyle choices to promote healthy aging, as well as vaccines and supplements that can enhance immune function and reduce the risk of infections and diseases.
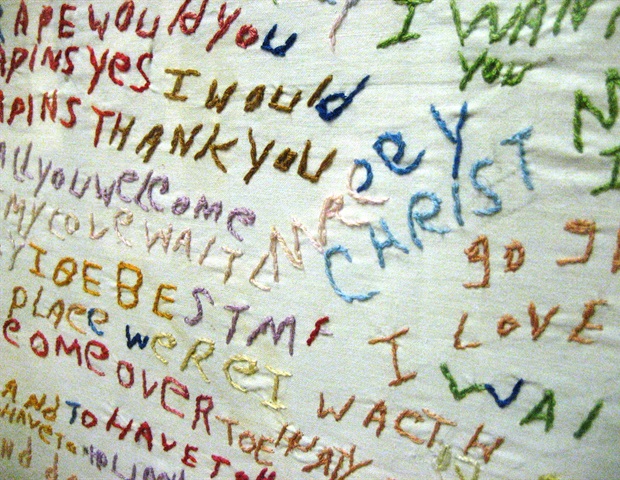
 Image Credit: meeboonstudio/Shutterstock.com
Image Credit: meeboonstudio/Shutterstock.com
You’ve been exploring how synaptic connections can be strengthened to combat neurodegenerative diseases. What broader impact could these findings have on future treatments for memory-related disorders?
Regulation of synaptic strength and communication is the basic mechanism underlying memory formation and storage.
Thus, by understanding the mechanisms underlying synapse formation and synaptic plasticity, we can delineate how deregulation of the process contributes to the pathogenesis of memory-related disorders. With improved understanding, we can then develop effective treatments for corresponding memory-related disorders.
In your work on drug discovery, including exploring compounds from traditional Chinese medicine, what potential do you see for these therapies to address global healthcare challenges in neurodegeneration?
Our drug discovery work has identified several novel molecular targets and a number of potential drug candidates with various mechanisms of action. Our exploration of traditional Chinese medicine (TCM) has also identified compounds or herbs with beneficial effects in AD.
TCM offers a wealth of promising drug candidates supported by its long history of use and extensive clinical data. We have sought to better understand the biological actions of the TCM herbs and their active compounds by evaluating their mechanisms of action in scientific model systems.
Some of the potential drug leads my lab has identified/developed show significant promise in treating AD. These are either in co-development with, or have been licensed for further development by, pharmaceutical companies. My lab has also pioneered a gene therapy technology for familial AD, which has been licensed for further development.
It should be noted that drug development is a long and arduous process, and it may be many years before treatments can be available for clinical use.
Drug development for AD is particularly challenging because AD is a complex, multifactorial condition involving different neuropathological mechanisms and multiple body systems. Developing effective therapies requires a thorough understanding of disease mechanisms.
Fortunately, in recent years, our understanding of AD and other neurodegenerative diseases has grown considerably. Global large-scale research collaborations are unraveling the complexities of these conditions, which have expanded disease targets for drug development.
Meanwhile, new technologies such as machine learning and artificial intelligence are streamlining and accelerating the drug development process. It is only a matter of time before we have additional disease-modifying treatments for AD and other neurodegenerative conditions.
As Alzheimer’s research progresses, how could new treatments targeting the immune system and brain health shift the way we prevent or manage the disease in the long term?
Traditionally, much of Alzheimer’s drug development efforts have focused on the two hallmark features of the disease: amyloid plaques and tau tangles. New understanding of the role of the immune system in AD is unveiling new molecular targets and new strategies for drug development, such as restoring impaired immune function in AD and addressing neuroinflammation.
This shift in focus will lead to the development of new classes of disease modifying treatments. For instance, therapies might target specific immune cells or pathways that contribute to neurodegeneration to mitigate the inflammatory processes that exacerbate cognitive decline.
Immune-targeted strategies could also be used alongside existing drugs to provide comprehensive treatment options that both alleviate symptoms and modify disease trajectory.
With rapid advances in brain science, how do you see new technologies shaping the future of neuroscience research and treatment approaches?
New advances are shaping brain research in very exciting ways. They are deepening our understanding of the brain as well as brain diseases and disorders at a rapid pace, and accelerating progress in the development of new treatments and therapies. For instance, advances in neuroimaging are providing unprecedented insights into brain activity and connectivity.
New technologies are also helping to reveal the biological changes in brain cells at a single-cell level and within a spatial context. This advancement is helping us delineate the pathological mechanisms of AD in greater detail.
Other advances include innovative genetic and molecular tools such as CRISPR and other gene-editing technologies to manipulate genes linked to neurological disorders, which could lead to targeted therapies for conditions such as familial AD.
Meanwhile, machine learning and artificial intelligence are helping researchers analyze vast amounts of neuroimaging and genetic data, identify patterns, and develop predictive models to further aid and accelerate research efforts.
As you work on the frontlines of neuroscience innovation, what upcoming developments in the field do you believe will have the greatest impact on society?
We are excited about a number of upcoming developments. The first is early diagnosis of AD – identifying patients when the disease is still in its early stage and treatable.
Currently, AD is primarily identified through cognitive assessments but by the time cognitive decline is evident, the disease has progressed to an advanced stage. Early diagnosis is a game-changer, allowing for timely clinical interventions that can lead to better treatment outcomes, thus improving the quality of life for patients.
The second is the ability to stratify AD patients into disease subtypes for development of precision medicine approaches. This will help identify suitable candidates for targeted drug treatment in clinical trials with specific disease-modifying drugs.
With precision medicine, patients will receive tailored treatments based on their individual genetic profiles and disease subtypes, resulting in better treatment outcomes with fewer side effects. The knowledge of an individual’s disease profile will also help refine patient selection for clinical trials. Only those likely to benefit from a treatment will be included, thereby improving trial outcomes. This approach will accelerate AD drug development and streamline the process for gaining FDA approval, ensuring that effective treatments reach patients more quickly.
Third, we are continuously deepening our understanding of the pathological mechanisms of AD to facilitate identification of promising therapeutic targets and drug leads to expand the range of potential therapeutic approaches for the disease.
Together, these efforts hold great promise for improving the diagnosis, treatment, and overall management of Alzheimer’s disease, leading to better outcomes for patients and their families.
Looking ahead, how do you hope your research will influence the future of Alzheimer’s disease treatment and broader brain health initiatives?
I hope my work enables early diagnosis and leads to the development of effective disease modifying treatments and precision medicine approaches. All of these will greatly enhance disease management as patients will be able to receive timely treatment tailored to their specific needs.
Over the long term, a holistic approach towards AD management is needed. This includes increased awareness of brain health and encouraging individuals to prioritize cognitive wellness throughout their lives.
By educating people on the importance of early detection and adopting healthy lifestyles, we can empower them to take proactive steps in maintaining their brain health, potentially reducing the personal and societal impact of AD.
Where can readers find more information?
- The Hong Kong University of Science and Technology – Study in The Hong Kong University of Science and Technology |Guangdong-Hong Kong-Macao Greater Bay Area|HKUST
- Nancy Ip’s lab homepage – Ip Lab – Molecular Neuroscience Laboratory (hkust.edu.hk)
- Hong Kong Center for Neurodegenerative Diseases – https://www.hkcend.org/
About Nancy Yuk-Yu IP, PhD
 Nancy Y. IP is the President of The Hong Kong University of Science and Technology (HKUST) and the Morningside Professor of Life Science. Taking office in October 2022, she is the first female president of a publicly funded university in Hong Kong.
Nancy Y. IP is the President of The Hong Kong University of Science and Technology (HKUST) and the Morningside Professor of Life Science. Taking office in October 2022, she is the first female president of a publicly funded university in Hong Kong.
Ip received her PhD degree in Pharmacology from Harvard University, after which she held the position of Senior Staff Scientist at Regeneron Pharmaceuticals Inc. in New York. Since joining HKUST in 1993, she has served as the Vice-President for Research and Development, the Dean of Science, and the Head of Biochemistry.
Ip is world-renowned for her significant contributions to the field of neuroscience in understanding the complex mechanisms that underlie proper brain functions, as well as drug discovery for neurodegenerative diseases. Her outstanding research has resulted in over 330 scientific papers and 70 patents. A distinguished neuroscientist, Ip is an elected member of the Chinese Academy of Sciences, the US National Academy of Sciences, and the American Academy of Arts and Sciences, among other academies, and is a recipient of numerous awards and honors, including the National Natural Science Awards, the L’OREAL-UNESCO for Women in Science Award and the 10 Science Stars of China by Nature.
As a distinguished neuroscientist, Ip helps shape research policy on a global level. She is a member of various strategic initiatives such as the Leadership Group of the Davos Alzheimer’s Collaborative. Additionally, she actively serves on local committees, such as the Chief Executive’s Council of Advisers, to help steer the strategic development of Hong Kong. She is also frequently invited to serve on many prominent organizations. For example, she was the first international member elected to the Council of the Society for Neuroscience, the Senior Editor of the Journal of Neuroscience, and a member of the WEF Global Agenda Council on Brain Research, Global Future Council on the Future of Neurotechnologies and Brain Science, Dana Alliance for Brain Initiatives, APEC Policy Partnership on Science, Technology and Innovation, and IBRO Asia Pacific Region Committee.
More from SfN 2024: How the Arts Reshape Brain Function: Susan Magsamen on the Future of Neuroaesthetics