In a recent study published in the Journal Nutrients, researchers investigated the effects of vitamin D/iron statuses and calcium intake on lumbar cortical and trabecular bone in male adults aged 15-19.
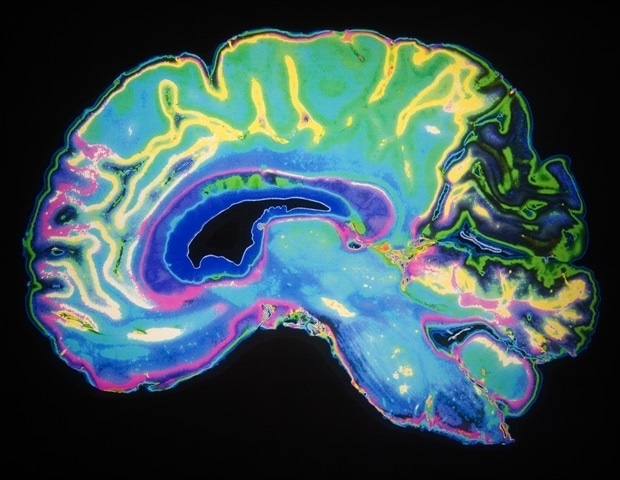
 Study: The Relationship between Bone Health Parameters, Vitamin D and Iron Status, and Dietary Calcium Intake in Young Males. Image Credit: Tatjana Baibakova/Shutterstock.com
Study: The Relationship between Bone Health Parameters, Vitamin D and Iron Status, and Dietary Calcium Intake in Young Males. Image Credit: Tatjana Baibakova/Shutterstock.com
Background
There are several knowledge gaps in research on the effects of nutrients on bones. First, research has focused only on the cortical part of the bones or their metabolism, not the trabecular.
Second, the results from studies (most done using animal models) investigating the effects of micronutrients, for instance, vitamin D, on trabecular bone structure need to be clarified.
Third, the little research done on human subjects has focused on the elderly population, which is why it remains obscured how the availability of some nutrients is essential for maintaining a healthy skeleton in adults and for bone growth and development across childhood.
Another challenge with research on the exclusive effects of vitamin D on bone health is that most have relied on computed measures of a total of 25(OH)D in serum instead of the free fraction of 25(OH)D; the latter is a superior measure of vitamin D status for bone health.
Furthermore, despite evidence of a cause-and-effect relationship between vitamin D (with calcium) and the risk of low-trauma bone fractures, the relationship between vitamin D status and bone mineral density (BMD) remains ambiguous.
Finally, data on the association between iron deficiency (ID) and bone health are limited.
About the study
In the present study, researchers analyzed data from 113 young male subjects who met the following criteria: i) aged between 15-19; ii) engaged in some osteogenic sports (volleyball or ski jumping) or were non-athletes (constituted the control group); iii) did not suffer from any injury across the 12 months before the study; iv) had body mass index (BMI) below 15 kg/m2 and above 37 kg/m2; and v) provided informed consent.
Of these 113 participants, 76 were from Polish national youth ski jumping and volleyball teams (28 ski jumpers, 48 volleyball players), and 37 were non-athletes.
The team obtained the bone densitometry, lumbar spine bone mineral apparent density (BMAD), and trabecular bone score (TBS) measurements using dual-energy X-ray absorptiometry (DXA).
Additionally, they evaluated body iron stores (Fe_S) based on serum ferritin and soluble transferrin receptor (sTfR) levels.
Furthermore, they determined each participant’s dietary calcium intake using a semi-quantitative food frequency questionnaire.
Results
The results confirmed a positive relationship between BMAD and Z-score and the vitamin D serum levels, with the association being stronger for the free fraction 25 (OH) D than the commonly used total fraction.
Free 25(OH)D explained 25% of the total 32% of BMAD variation in the lumbar spine measurements of the sports group.
It is noteworthy here that the free fraction constitutes only 0.1–2% of the total hydroxy vitamin D in the human body, while the remaining circulates in the blood bound to albumin and mainly with vitamin D-binding proteins (VDBPs), implying, at least theoretically, that the relationship between both should be comparable across all individuals.
However, in this study, the correlation between these two fractions in the athletes was lower than controls (0.77 vs. 0.93). Therefore, the authors presumed that physical exercise affects the total hydroxy vitamin D fraction by influencing the VDBP levels.
Further, the authors noted that 22% and 15% of the athletes and controls, respectively, were iron-deficient.
While their ferritin and iron stores simultaneously correlated with BMAD, no such correlation emerged with the Z-score in the sports group, which, to some extent, was attributable to the lack of adjustment of the Z-score to height.
Of the total 32% of BMAD variation observed in the lumbar spine measurements of the sports group, 7% was explained by ferritin, suggesting it is a more reliable indicator of bone mineralization in athletes than the calculated iron stores.
Furthermore, the usual calcium intake did not impact BMAD in both groups. As the observed total fraction of 25(OH)D was low in both groups, it could have modulated calcium absorption in the gut.
During puberty, high calcium retention efficiency likely compensates for low calcium intake.
However, prolonged vitamin D deficiency (even moderate) in adulthood may severely impair dietary calcium absorption in the gut, resulting in increased bone loss.
The authors found no relationship between the nutritional factors analyzed in this study and the trabecular structure of bones.
Even though both BMAD and Z-score correlated with the TBS in the controls, the correlation coefficients differed, while no such correlation existed in the sports group.
Moreover, the “Fractures” factor was comparable in examined groups and independent of mineralization and TBS in the lumbar spine, suggesting that it may be independent of the level of physical activity and associated overloads.
Conclusions
The results of the present study confirmed the positive influence of normal vitamin D and iron status on cortical bone status in physically active athletes.
In their bone mineralization assessments, the free 25(OH)D fraction appeared as a better indicator than the total 25(OH)D and ferritin than calculated body iron stores.
Beyond nutritional factors, results suggested that their bone mineralization assessments should be adjusted-for-height BMAD, not raw aBMD data.
Furthermore, in these athletes, osteogenic physical exercises (e.g., jumps) also possibly affect trabecular bone.
Journal reference:
- Malczewska-Lenczowska, J.; Surała, O.; Granda, D.; Szczepańska, B.; Czaplicki, A.; Kubacki, R. (2024) The Relationship between Bone Health Parameters, Vitamin D and Iron Status, and Dietary Calcium Intake in Young Males. Nutrients 16, 215. doi: https://doi.org/10.3390/nu16020215.