In a recent study posted to bioRxiv preprint* server, researchers showed that transfer of immunoglobulin G (IgG) from long COVID patients causes symptoms in mice.
Evidence suggests that over 10% of coronavirus disease 2019 (COVID-19) survivors experience persistent symptoms beyond 12 weeks after recovery. This condition is known as long COVID-19 or post-COVID syndrome. However, its underlying pathophysiology is unclear. Several mechanisms have been proposed, linking long COVID symptoms to neuroinflammation, dysbiosis, dysregulated interferon response, cellular metabolism, and autoimmunity.
Studies indicate that autoimmunity is induced in acute and post-acute COVID-19. Long COVID-related autoantibodies bind to neurotransmitters, chemokines, G protein-coupled receptors, and immunomodulators. Clinical improvement in long COVID is likely associated with reduced autoantibodies. However, whether autoantibodies (actively) contribute to long COVID symptoms is unknown.
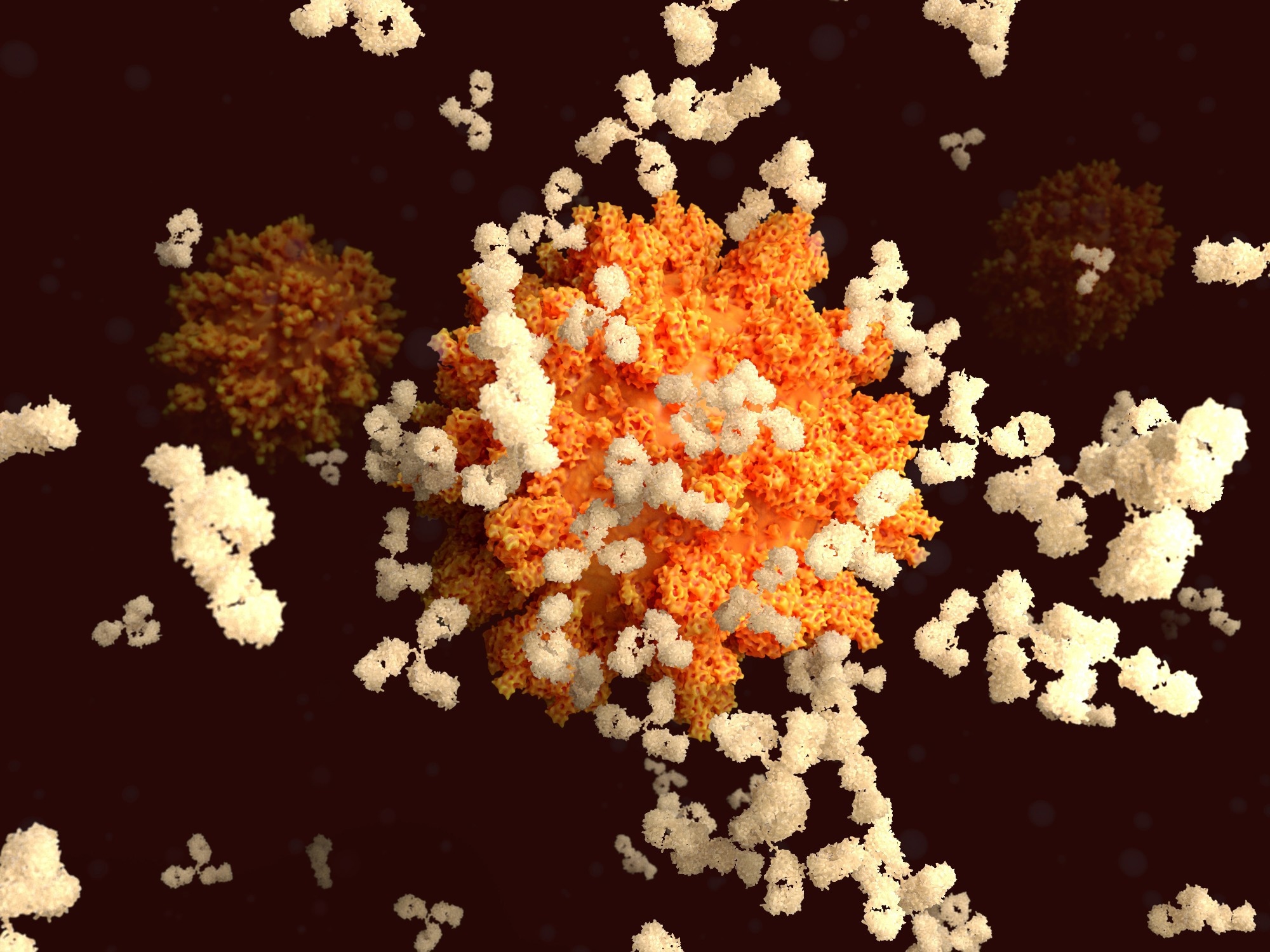 Study: Transfer of IgG from Long COVID patients induces symptomology in mice. Image Credit: Juan Gaertner / Shutterstock
Study: Transfer of IgG from Long COVID patients induces symptomology in mice. Image Credit: Juan Gaertner / Shutterstock




The study and findings
In the present study, researchers evaluated the role of autoantibodies in long COVID pathogenesis. They included long COVID-19 patients aged 18–65 attending a post-COVID-19 clinic in Amsterdam. Blood samples were obtained at least 90 days post-infection. Data on demographics, symptoms, comorbidities, and medications were obtained from health records.
Two control groups were included – healthy subjects sampled before the pandemic and healthy individuals after mild COVID-19 without residual symptoms. Assays were performed to quantify interleukin (IL)-10, IL-6, IL-1β, IFN-β, IFN-γ, IFN-α2a, total tau, glial fibrillary acidic protein (GFAP), and neurofilament L (NFL) in the plasma of long COVID patients and controls. Olink proteomics technology was used for protein profiling.
IgG antibodies were purified from patients and controls. Further, adult C57BL/6 mice were injected with IgG, and behavioral tests were performed. The Hargreaves and von Frey tests determined heat withdrawal latency times and mechanical thresholds, respectively. An open field test examined locomotor activity while the rotarod analysis determined stamina. Next, murine tissues were harvested for immunohistochemistry.
Findings
In total, 34 long COVID patients were included; they had confirmed SARS-CoV-2 infection and were in good mental and physical health pre-COVID-19. They were not hospitalized, and their symptoms lingered for at least six months post-infection. Patients experienced diverse symptoms, but fatigue was consistent. Twenty-six patients were unable to resume occupational roles, 25 reported pain, and 29 experienced post-exertional malaise.
In addition, 15 healthy controls with a mild infection were included. Pro-inflammatory cytokines in acute COVID-19 were comparable between long COVID patients and controls. IFN-γ was lower in long COVID patients, while IFN-β was elevated. GFAP, detected in 10 long COVID patients, was elevated; it was undetectable in controls. No significant differences were observed in tau and NFL levels between controls and long COVID patients.
The team stratified long COVID patients based on IFN and GFAP levels; the long COVID-1 (LC-1) group comprised 12 patients with increased levels of astroglia activation and neuronal damage markers. LC-2 comprised 10 patients with increased type 1 IFNs (IFN-β and IFN-α2a) compared to LC-3. LC-3 had lower levels of IL-1β, IL-6, type 1 IFNs, and TAU than LC-2.
IFN-γ levels were not different between subgroups. Partial least-squares discriminant analysis showed that LC-1 separated on principal component 1 (PC1), while the others segregated on PC2. Subsequently, gene set enrichment analysis was performed; this indicated that LC-1 was associated with higher levels of intracellular transport proteins and lower levels of cell surface proteins.
In contrast, LC-2 was enriched for muscle-related proteins, whereas LC-3 was enriched for lipoproteins. Purified IgG from long COVID patients and healthy controls sampled pre-pandemic were pooled and injected into mice. Fifteen days later, the presence of the human IgG (hIgG) in various tissues was investigated. Overall, hIgG from patients or controls was detected in all investigated tissues at similar levels in mice.
Long COVID IgG recipients exhibited a reduced mechanical sensory threshold, indicating mechanical hypersensitivity compared to controls. LC-1 hIgG recipients developed this mechanical hypersensitivity on day 3, while LC-3 hIgG recipients developed 24 hours post-administration. However, latency to heat stimulation declined in all hIgG recipients, indicating elevated heat sensitivity.
This state normalized within three days in control hIgG recipients but persisted for up to 15 days in the LC groups. Mice injected with hIgG from long COVID patients exhibited a slight reduction in locomotor activity. Among subgroups, only LC-2 hIgG recipients had significantly lower walking distance on day 1 post-injection, while other LC groups showed no differences at any time points. No differences between LC and control hIgG recipients were observed in the rotarod analysis.
Conclusions
In sum, the results reveal at least three distinct long COVID subgroups. Passive transfer of IgG from these subgroups induced subgroup-specific pain-associated behavior and reduction in locomotor activity, suggesting a role of IgG in long COVID pathogenesis. Future studies should identify specific pathogenic IgGs for a more nuanced understanding of the disease and to develop targeted therapies.
A strong indication for #autoimmunity in #longcovid: transfer of antibodies of patients induces symptoms in mice. Check out our latest preprint @biorxivpreprint: https://t.co/c9I3ZKEEIF 1/11
— Jeroen den Dunnen (@DrDenDunnen) June 1, 2024










;Resize=(1200,627)&impolicy=perceptual&quality=medium&hash=4a0b4b14d56d88e85cb3ef2625c61b429dceebcbe71d8543ec8099449b40f08e)
