Using high-resolution retinal images, a novel AI model detects Alzheimer’s disease and mild cognitive impairment early, offering hope for more timely, noninvasive, and affordable dementia care.
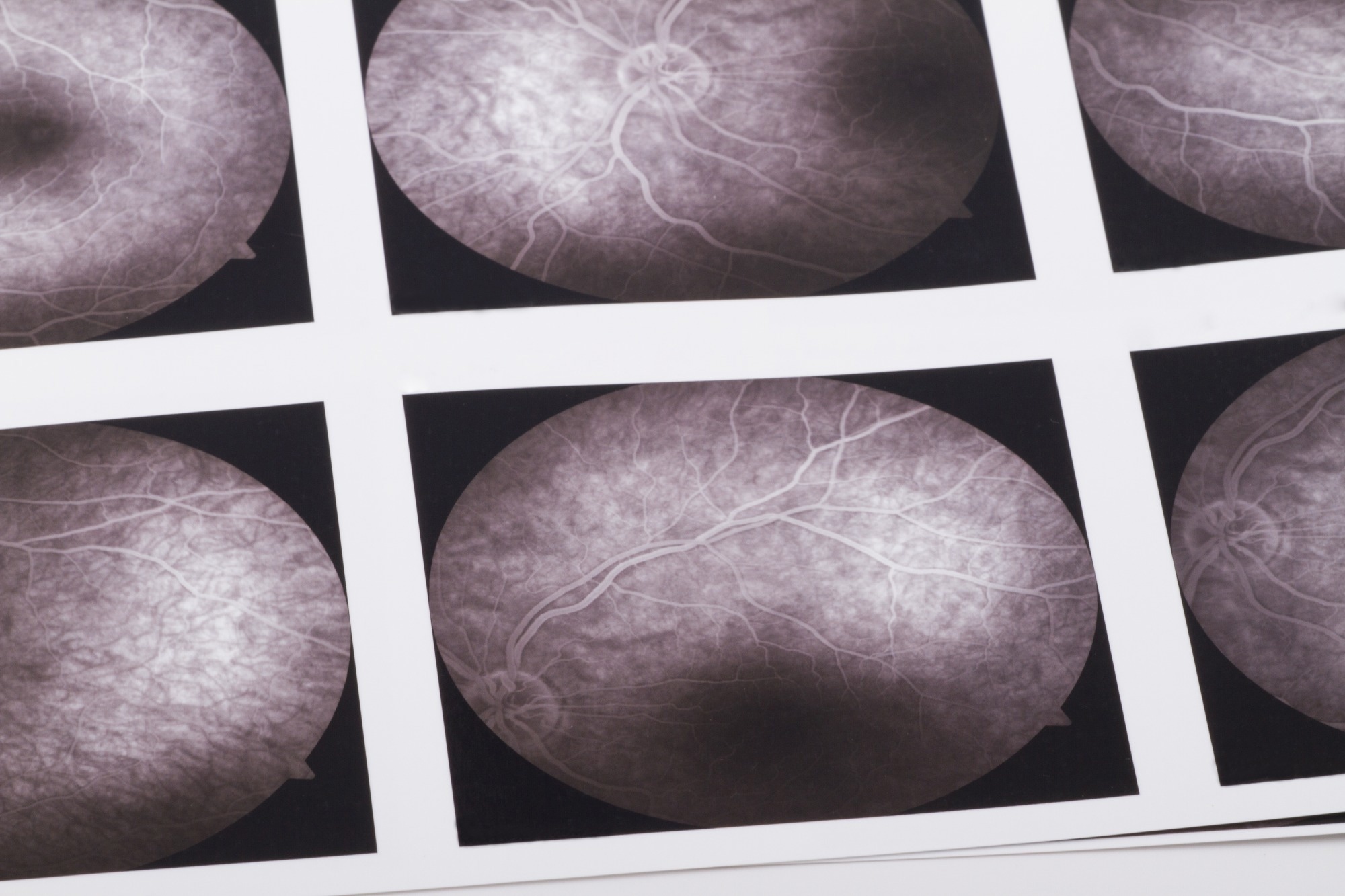 Study: Early detection of dementia through retinal imaging and trustworthy AI. Image Credit: bfk / Shutterstock
Study: Early detection of dementia through retinal imaging and trustworthy AI. Image Credit: bfk / Shutterstock
In a recent study published in the journal NPJ Digital Medicine, researchers have developed a deep learning algorithm capable of analyzing high-resolution images of retinal vasculature to detect Alzheimer’s disease (AD) and mild cognitive impairment (MCI) at early stages. This innovative approach could enable clinicians to identify patients with a high risk of dementia, allowing timely pharmacological intervention to slow the progression of the disease and its detrimental effects.
The study, which utilized 5,751 images from 1,671 participants, revealed that this new method significantly outperformed conventional AD and MCI detection techniques. Not only is it accurate, but the method is also inexpensive, fast, and entirely noninvasive, making it ideal for widespread screening. Researchers suggest that further validation of this approach could revolutionize dementia care by enabling early detection and management on a large scale.
Background
Dementia is a progressive condition that primarily affects cognitive functions, including memory, information processing, and reasoning, leading to a decline in the ability to perform everyday tasks. Recent advancements in medicine have extended human lifespans, contributing to a global surge in dementia cases, which now affect over 50 million people and is expected to rise in the coming years.
Despite extensive research, existing methods for detecting dementia, including biochemical tests and magnetic resonance imaging (MRI), are limited by high costs, invasiveness, and the need for specialized facilities. Moreover, these techniques often fail to detect early-onset Alzheimer’s disease (EOAD), limiting the ability to intervene in high-risk individuals early.
Recent research has highlighted a potential link between the retina—often referred to as the “window to the brain”—and neurodegenerative diseases like AD. Clinical studies and histopathological reports have demonstrated unique microvascular changes in the retina among AD patients. These findings have spurred interest in using advanced ophthalmic imaging techniques, such as optical coherence tomography angiography (OCTA), to identify retinal biomarkers associated with cognitive decline.
OCTA is a state-of-the-art imaging technique that allows for rapid and noninvasive imaging of the retinal microvasculature, including even the smallest capillaries with a resolution of 5–6μm. This technology provides detailed insights into the microvascular network and the structure of the foveal avascular zone across different retinal layers, as well as the choroid.
By leveraging OCTA data in conjunction with artificial intelligence (AI), researchers aim to create a cost-effective and scalable solution to identify individuals at risk for dementia, promote healthy aging, and facilitate timely interventions.
About the Study
In this study, the researchers developed and tested a novel deep-learning model called “Eye-AD.” The model was specifically designed to analyze OCTA images and identify patients with early-onset Alzheimer’s disease or mild cognitive impairment. The model processes high-resolution data from various retinal layers, including the superficial vascular complex (SVC), deep vascular complex (DVC), and choriocapillaris (CC), to detect patterns associated with cognitive decline.
The study data was collected from two primary cohorts—ROMCI (Retinal OCTA-based MCI detection) and ROAD (Retinal OCTA-based EOAD detection)—which comprised retinal images centered on the fovea. The images captured information on the retina’s vascular structures, providing the dataset for model training and evaluation.
The Eye-AD model comprises two main parts: a convolutional neural network (CNN) for feature extraction and a graph neural network (GNN) for final prediction. These components work together to analyze the intricate relationships between retinal layers, enabling a more comprehensive evaluation of cognitive function. The model was tested with multiple encoders, including ResNet and ConvNeXt, and ConvNeXt was ultimately selected due to its speed and consistent performance.
Study Findings
The study’s results indicate that the Eye-AD model is highly accurate and reliable. Its performance exceeded that of traditional biochemical and MRI-based detection methods, with an AUC (Area Under the Curve) of 0.9355 for detecting EOAD and 0.8630 for MCI. The model’s strength lies in its accuracy, cost-effectiveness, and ability to process data quickly, making it a practical option for large-scale screening.
The model’s interpretability analysis also highlighted that the deep vascular complex (DVC) played a more critical role in detecting EOAD and MCI than the other retinal layers, suggesting that deeper retinal structures may be more affected by cognitive decline. Specifically, the DVC was found to contribute more to the model’s predictions, with an average importance score of 40% and 49% for EOAD and MCI cases, respectively. These findings suggest that changes in the deeper retinal layers could provide insights into the mechanisms underlying dementia and its progression.
Moreover, the study showed that differences in retinal structure were more pronounced in patients with EOAD than those with MCI, likely reflecting the more severe impact of Alzheimer’s disease on the retinal vasculature. These findings support the hypothesis that dementia-related changes are more detectable in the deeper layers of the retina.
Conclusion
The Eye-AD model represents a significant advancement in the early detection of dementia. Its ability to noninvasively screen large populations using only high-resolution retinal images makes it an ideal tool for widespread cognitive health assessments. The model is not only accurate but also deployable at scale, making it possible to identify individuals with early-stage Alzheimer’s disease or MCI and facilitate timely interventions.
While the model has shown great promise, the researchers emphasize the need for further studies to validate its performance across more diverse populations. Integrating other modalities, such as blood tests or cognitive assessments, could also enhance the model’s diagnostic power. With continued development, the Eye-AD model has the potential to become a valuable resource for dementia screening and monitoring in the future, promoting healthier aging and improving patient outcomes.




_labeled_with_fluorescence_dyes-Vshivkova_9fc952884c46485589d5e3d9bff007e5-620x480.jpg)

