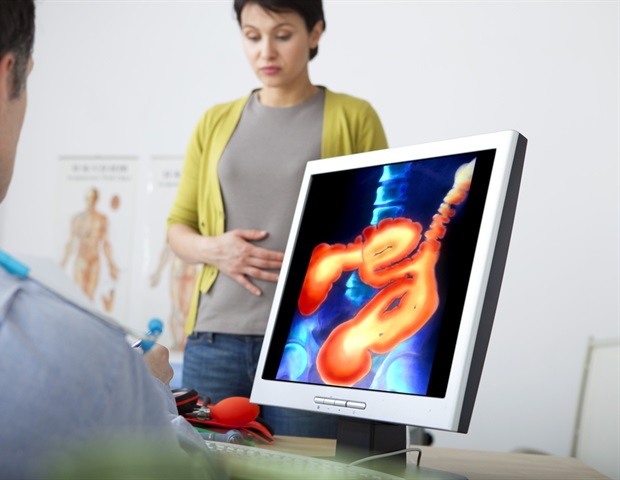
Patients with suspected inflammatory bowel disease (IBD) could benefit from better testing protocols that would reduce the need and lengthy wait for potentially unnecessary colonoscopies, a new study has found.
In a paper published in Frontline Gastroenterology, researchers from the Birmingham NIHR Biomedical Research Centre (BRC) at the University of Birmingham tested a new protocol to improve IBD diagnosis combining clinical history with multiple home stool tests.
In the two-year study involving 767 participants, patients were triaged and had repeated fecal calprotectin (FCP) tests and the research team found that the use of serial FCP tests were able to strongly predict possible IBD as well as Crohn’s Disease and Ulcerative Colitis.
The team observed that a second FCP test was a strong indicator of a potential need for further investigation including colonoscopy; although the researchers observed that only 20% of patients had two samples submitted prior to referral to secondary care.
Dr Peter Rimmer from the Birmingham NIHR Biomedical Research Centre at the University of Birmingham and corresponding author of the study said:
“Patients who experience symptoms associated with inflammatory bowel diseases often have a long wait until getting a diagnosis, and current testing is under immense strain.
“Using a comprehensive 13-point symptom checker and multiple FCP tests, we have been able to identify much more accurately patients who had IBD and other diseases. The rollout of this protocol could reduce the time taken to get a diagnosis and start treatment for IBDs as much more of the screening and testing can be done through primary care. The sensitivity of multiple FCP tests can be used to flag those patients who urgently need referral into secondary care.”
In its simplest form, this study may help improve referral triage for IBD patients. But as we plan new care pathways, it could open up new exciting possibilities: with the growing availability of home FCP testing, these tests’ results combined with simple symptom questionnaires could feed into algorithms that allow patients to self-refer to secondary care services, reducing strain on primary care. This is something we’re going to explore in a large follow-up study we’re currently initiating.”
Dr Rachel Cooney, Consultant Gastroenterologist at University Hospitals Birmingham NHS Foundation Trust, researcher at the NIHR Birmingham BRC and co-author of the study
Source:
Journal reference:
Rimmer, P., et al. (2024). Optimising triage of urgent referrals for suspected IBD: results from the Birmingham IBD inception study. Frontline Gastroenterology. doi.org/10.1136/flgastro-2023-102523.