Even as they have revolutionized the treatment of certain forms of cancer, CAR T-cell therapies have been shadowed by a significant limitation: many patients, including those whose cancer goes into full remission, eventually relapse. In a new study, Dana-Farber Cancer Institute researchers report on a technique with the potential to eliminate that problem.
The approach, described in a paper published online today in the journal Nature Biotechnology, works by spurring CAR T cells to be more active and persist longer in the body, enabling them to remain in battle mode until all tumor cells are eliminated. The technique – creates what researchers dub a CAR-Enhancer (CAR-E) therapeutic platform – also causes CAR T cells to form a memory of the cancer cell, so they can spring back into action if the cancer recurs.
In experiments in patient-derived laboratory cancer cell lines and other studies, CAR-Enhancer treatment succeeded in eradicating all tumor cells, clearing the way for clinical trials of this approach in human patients. Researchers hope to launch the first trial in the near future.
“CAR T-cell therapies have been a breakthrough treatment for B-cell hematologic cancers such as B-cell leukemias and lymphomas and multiple myeloma,” says the study’s senior author, Mohammad Rashidian, PhD, of Dana-Farber.
In myeloma, for example, virtually 100 percent of patients have an excellent response to CAR T-cell therapies initially, but almost all relapse, half of them within one to two years of treatment. Relapse coincides with the disappearance of CAR T-cells in the bloodstream.”
Mohammad Rashidian, Dana-Farber Cancer Institute
“Most of the research to address this challenge has focused on re-engineering the CAR T cell itself – for example, by introducing or eliminating genes to keep the cell active for longer,” he continues. “While these approaches hold great promise, they have yet to show much effectiveness in the clinic. We decided to come at the problem from a completely different perspective.”
Instead of trying to alter the inner workings of CAR T cells, Rashidian and his colleagues developed an approach that works from the outside – by delivering to the cells’ doorstep a molecule that extends their lives and prompts them to form memory. The vehicle for accomplishing this is a fused-together “platform” unlike any other used in medical treatment.
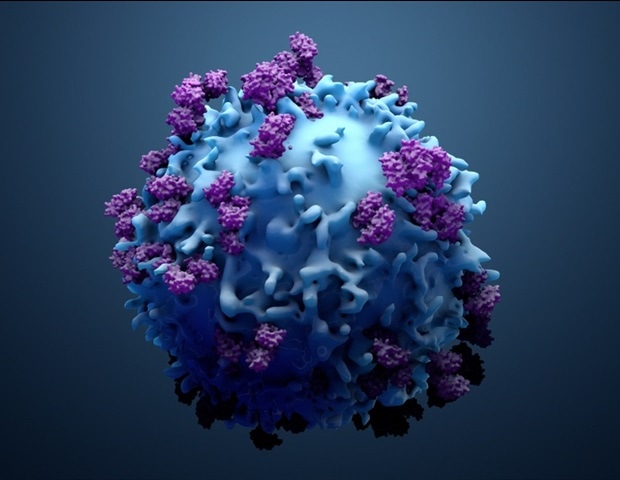
CAR T cells are genetically enhanced versions of a patient’s own cancer-fighting T cells. They’re made by removing a few million T cells from a patient’s blood and genetically equipping them to produce a special structure, called a chimeric antigen receptor, or CAR, on their surface. The CAR is designed to latch onto a specific marker, or antigen, on a patient’s tumor cells. The cells, now called CAR T cells, are grown in a lab until they number in the hundreds of millions. When the cells are infused back into the patient, their specially designed receptor locks onto the tumor cell antigen and triggers an immune system attack on the cancer.
“The attack destroys nearly all the tumor cells, but a tiny percentage remains,” Rashidian explains. “The CAR T cells are effector cells: they live to kill cancer cells. When they can’t find any more to kill, they act as if their job is done and go away. The remaining tumor cells, however, can set the stage for a resurgence of the cancer.”
To prolong the CAR T cells’ assault and endow them with memory, the Dana-Farber researchers developed a completely novel therapeutic agent, the CAR-E platform. It consists of a weakened form of the immune-signaling molecule interleukin-2 (IL-2) fused to the very antigen the CAR is designed to bind to.
“IL-2 has a strong effect on T cells – activating them and causing them to proliferate – but it can also be highly toxic to patients,” Rashidian remarks. “For that reason, we used a very weak form of it. On its own, it has no effect on normal T cells but has a stimulatory effect on CAR T cells when targeted specifically to them.”
That precision targeting is accomplished by fusing IL-2 to a specific antigen. In CAR T-cell therapies for multiple myeloma, the CAR binds to an antigen called B-cell maturation antigen (BCMA) on myeloma cells. It is that antigen that is affixed to IL-2 in the new therapy.
“Just like weak IL-2, the BCMA antigen by itself doesn’t affect CAR T cells, but, together, they have a synergy whose impact was well beyond our expectations,” says the study’s first author Taha Rakhshandehroo, PhD, of Dana-Farber.
CAR-E therapy not only causes CAR T cells to proliferate but to diversify – to generate different types of CAR T cells with different properties – researchers found. “It generated not only effector T cells, which most patients already have, but also stem cell-like memory T cells, central memory T cells, effector memory T cells – a complete repertoire of the kinds of T cells needed for an effective immune response to cancer,” Rashidian remarks.
In laboratory cultures of myeloma cells and in animal models of the disease, CAR-E therapy brought about the complete clearance of tumor cells – an erasure of any sign of the cancer – researchers found.
There were other benefits as well. Researchers discovered that the long-lasting CAR T cells generated by the therapy could be re-stimulated by re-administering CAR-E. This suggests that patients who relapse after CAR T-cell therapy could be effectively treated with additional doses of CAR-E treatment. CAR-E also raises that possibility that patients could be treated with smaller numbers of CAR T cells than at present. The current practice of allowing CAR T cells to multiply into the hundreds of millions is a time-consuming, expensive, resource-heavy process that requires patients to wait many weeks before receiving an infusion of the cells. The large quantities are partly responsible for one of the most common side effects of CAR T-cell therapy: cytokine release syndrome, in which an over-aggressive immune response results in fever, nausea, rapid heartbeat, neurological problems or other issues. With CAR-E, it might be possible to skip the CAR T-cell expansion process altogether: CAR T cells would simply be made and infused into patients, followed by treatment with CAR-E.
“In animal studies, we infused mice with very low numbers of CAR T cells and found that weren’t able to clear the cancer,” Rashidian relates. “When we gave them the CAR-E treatment, the CAR T cells expanded and were able to clear the cancer.”
One of the first goals of a clinical trial of CAR-E therapy will be to ensure safety and to determine the best dose and schedule of administration. Initially, they expect that the treatment would begin about a month after patients are infused with CAR T cells. Treatment would consist of a weekly dose of CAR-E therapy for three or four weeks.
“The most exciting part of this therapy is how easily it can be integrated into the care of patients receiving CAR T-cell therapies,” Rakhshandehroo says. “It’s such an elegant solution to the problem of CAR T-cell depletion. We’re eager to begin testing it in clinical trials.”
Source:
Dana-Farber Cancer Institute