A recent study published in the Journal of Controlled Release demonstrated a novel method for delivering anti-cancer drugs conjugated to modified cell-penetrating peptides across the blood-brain barrier (BBB) in mice to treat glioblastoma (GBM).
Background
Like most tumors, brain tumors develop due to abnormal cell proliferation; they can be cancerous or non-cancerous. There are two types of primary brain tumors: glial (composed of glial cells) and non-glial (developing near nerves, blood vessels, or glands). Gliomas are brain tumors that originate from glial cells. Glioblastoma (GBM) is the most common, malignant (cancerous), and lethal of all glial tumors; most GBM patients live only for around 15 months after the diagnosis. The 5-year survival rate of GBM is below 5%.
A major challenge in treating brain cancer is the ability to transfer therapeutic agents through the BBB –, a network of blood vessels and cells that protects the brain from harmful substances. It has been observed that cancer-fighting drugs are unable to penetrate the BBB in therapeutic efficacious quantities. Drugs with proven anti-cancer efficacies do not show much of an effect on brain cancer outcomes, likely possibly owing to the selective penetrability of the BBB.
Standard cancer management involves surgical tumor excision, followed by radiation therapy and temozolomide (TMZ) chemotherapy. In the first year after the diagnosis, most patients will experience tumor recurrence. Cisplatin is commonly used to treat various types of tumors for its ability to destroy the deoxyribonucleic acid (DNA) by inter-or intra-strand crosslinks.
However, cisplatin and other platinum-based drugs are not considered effective for treating GBM as they cannot penetrate the BBB. Due to similar reasons, current anti-cancer drugs pose little therapeutic benefits to GBM patients. It has been proposed that enhancing BBB penetrability can be of enormous value as it could facilitate greater intra-tumoral drug concentrations.
It is possible to increase the amounts of drugs delivered to the GBM by using direct intraventricular injections and implantable drugs, such as Gliadel wafers, which can be directly inserted into the tumor-resection cavity immediately after surgery.
The BBB can be transiently made permeable using hyperosmotic solutions or targeted ultrasonography. Alternatively, non-invasive central nervous system (CNS)-delivery methods are promising, and several such modalities currently undergoing preclinical trials. Among these are nanoparticles that penetrate the BBB, liposomal formulations, and peptide-based delivery systems, for example, cell-penetrating peptides (CPPs).
Peptides conjugated with drugs are emerging as important therapeutic agents in treating various diseases, including cancer. Peptides are efficacious in brain tumors as they peptides harbor an inherent ability to cross membranes and penetrate tissues.
Previously, the researchers created M13 – a CPP Transportan 10 (TP10) derivative, which was synthesized by adding a perfluoroaryl macrocycle to the latter. This change enables greater penetrability through the three-dimensional BBB spheroids in vitro and causes accumulation in the mouse brain in vivo. Pt (IV)-M13 facilitates platinum transport into the brain tissue of healthy mice, following conjugation to cis,cis,trans-[Pt (NH3)2Cl2(OH)2], a Pt(IV) prodrug form of cisplatin.
Platinum is easily detectable by inductively-coupled plasma mass spectrometry (ICP-MS) – a technology that can quantify minuscule levels of metals in biological tissue.
The study
In the current study, researchers examined the transport of platinum by the Pt(IV)-M13 combination in a BBB-spheroid model, in vitro, as well as in the healthy brain and tumor of a mouse GBM-xenograft model.
Here, preparation and initial characterization of drug-conjugated peptide [Pt(IV)-M13] were performed. The cytotoxicity of Pt(IV) was evaluated by comparing its effects on GBM cell lines cultured as neurospheres with those of Pt(IV) without conjugation and cisplatin. A three-dimensional BBB spheroid model that simulates the BBB was used to analyze, in vitro, the penetration of drugs and peptides across the BBB.
A quantitative analysis of the platinum amounts in GBM-tumor-bearing mice was performed using ICP-MS to determine platinum’s BBB-penetrating properties and biodistribution.
Pt(IV)-M13 conjugate was administered to tumor-bearing nude mice to examine the pharmacokinetics of platinum accumulation in healthy brain and tumor tissues. ICP-MS analysis of brain tissue and tumor tissue was conducted over time. A reference constant dosing schedule of 5 mg/kg of cisplatin was chosen to evaluate the drug-conjugated peptide’s pharmacology.
Drug-conjugated peptides were analyzed using confocal immunofluorescence microscopy to detect the DNA damage marker – γH2AX. Concurrent administration of Pt(IV) prodrugs with cisplatin was undertaken at the maximum tolerated dose (MTD) of 5 mg/kg – with increasing doses.
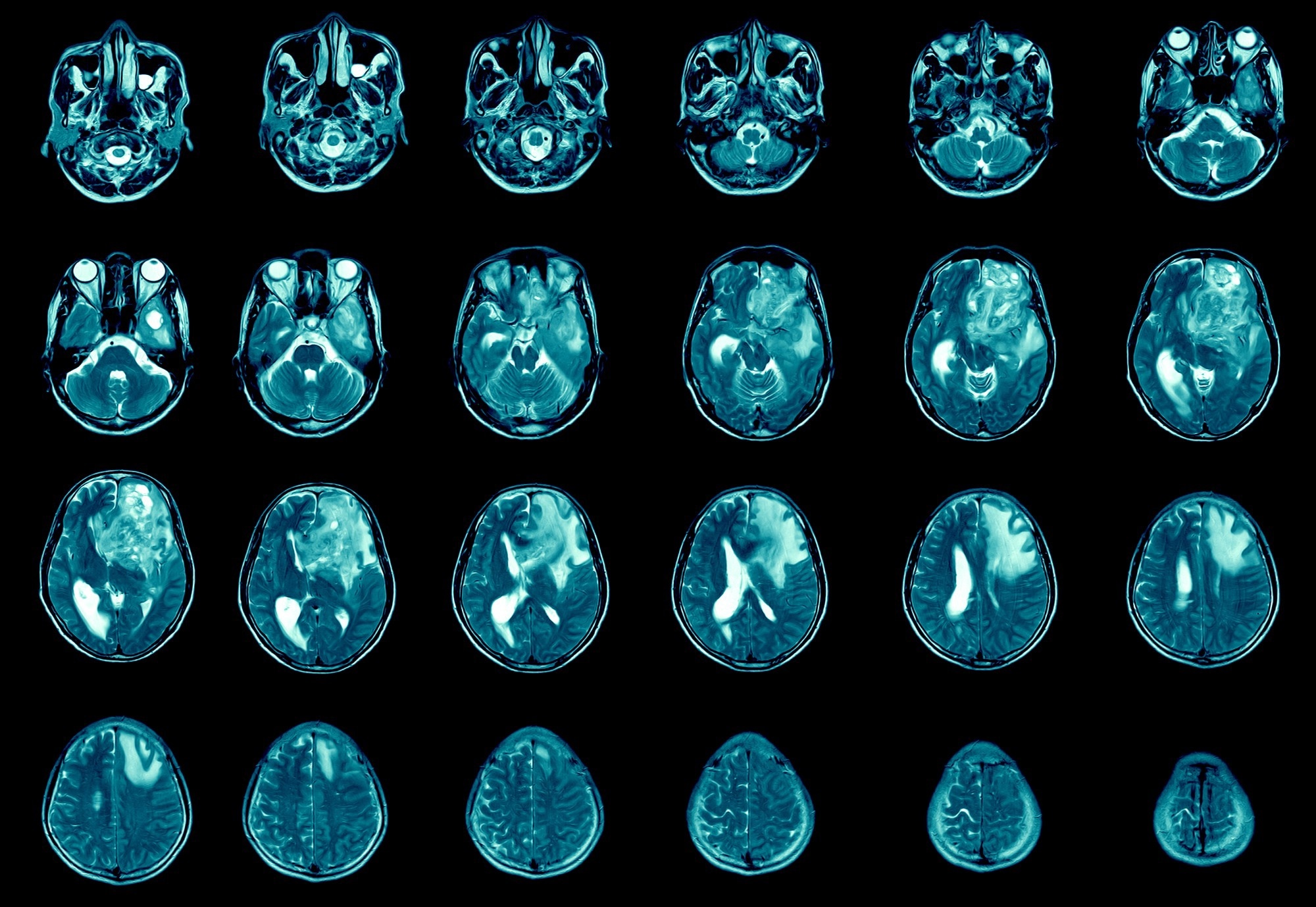
Using a four-week treatment schedule with an initial dose of 5-30 mg of the drug-conjugated peptide, the effects at its highest tolerated dose (15 mg/kg, twice weekly) on tumor growth in the GBM animal models were evaluated. Researchers conducted an MRI study during therapy (20 days post-tumor implantation) to compare tumor growth behavior between groups as the control group began to reach predetermined growth targets.
Findings
It was found that when compared to Pt(IV) alone, conjugation of the Pt(IV) prodrug to the M13 peptide significantly increased the cytotoxicity of Pt(IV) and decreased neurosphere growth in GBM cell lines. It was demonstrated in vitro that the drug-conjugated peptide killed GBM cells effectively.
Further, platinum absorption was limited in BBB spheroids treated with cisplatin or Pt(IV) prodrugs alone. However, platinum absorption increased in the BBB spheroid model when Pt(IV) prodrugs were conjugated with M13 peptides. This implied that the drug-conjugated peptide efficiently transited the BBB spheroids.
Drug-conjugated peptide treatment significantly increased platinum uptake compared to cisplatin in healthy brain tissue and eight-fold in tumor tissue. According to this study, conjugating M13 to a Pt(IV) prodrug resulted in enhanced platinum uptake across the BBB and elevated platinum concentrations in the brain and tumor. Meanwhile, the lungs and kidneys, the primary sites of platinum-drug accumulation, did not show any significant differences.
Five hours following injection of the drug-conjugated peptide Pt(IV)-M13, platinum accumulation in the healthy brain and tissue reached its maximum. No significant weight gain was associated with administering the drug-conjugated peptide. The data also found that mice tolerate increased dosages of Pt(IV)-M13 well.
Further, neither the dose nor the time-point showed significant differences, indicating that these doses are safe for nude mice and appropriate for exploratory survival studies.
It was also found that elevated platinum levels, when combined with Pt(IV)-M13 treatment enhanced DNA damage in tumors, which is believed to contribute to the observed improvement in survival. The authors demonstrated, for the first time, that coupling a cisplatin prodrug (Pt(IV)) to a macrocyclic cell-penetrating peptide (M13) was effective.
These results indicated that conjugation of cisplatin with a macrocyclic cell-penetrating peptide (M13) enables effective dosing in mice – at three times higher MTDs than cisplatin alone, thus, conferring significant survival advantages.
Conclusion
The results elucidated that systemic injection of a Pt(IV) complex conjugated to a brain-penetrant macrocyclic peptide can accentuate the brain-platinum levels and extend survival in mouse GBM models.
Perfluoroaryl macrocyclic-stapled CPPs show promising outcomes when used as drug delivery vehicles for trans-BBB brain tumor treatment. Further, Pt(IV)-M13 is a promising strategy for the systemic delivery of GBM chemotherapeutics to the brain, which overcomes the challenges posed by the BBB, which currently impedes most oncological therapies.