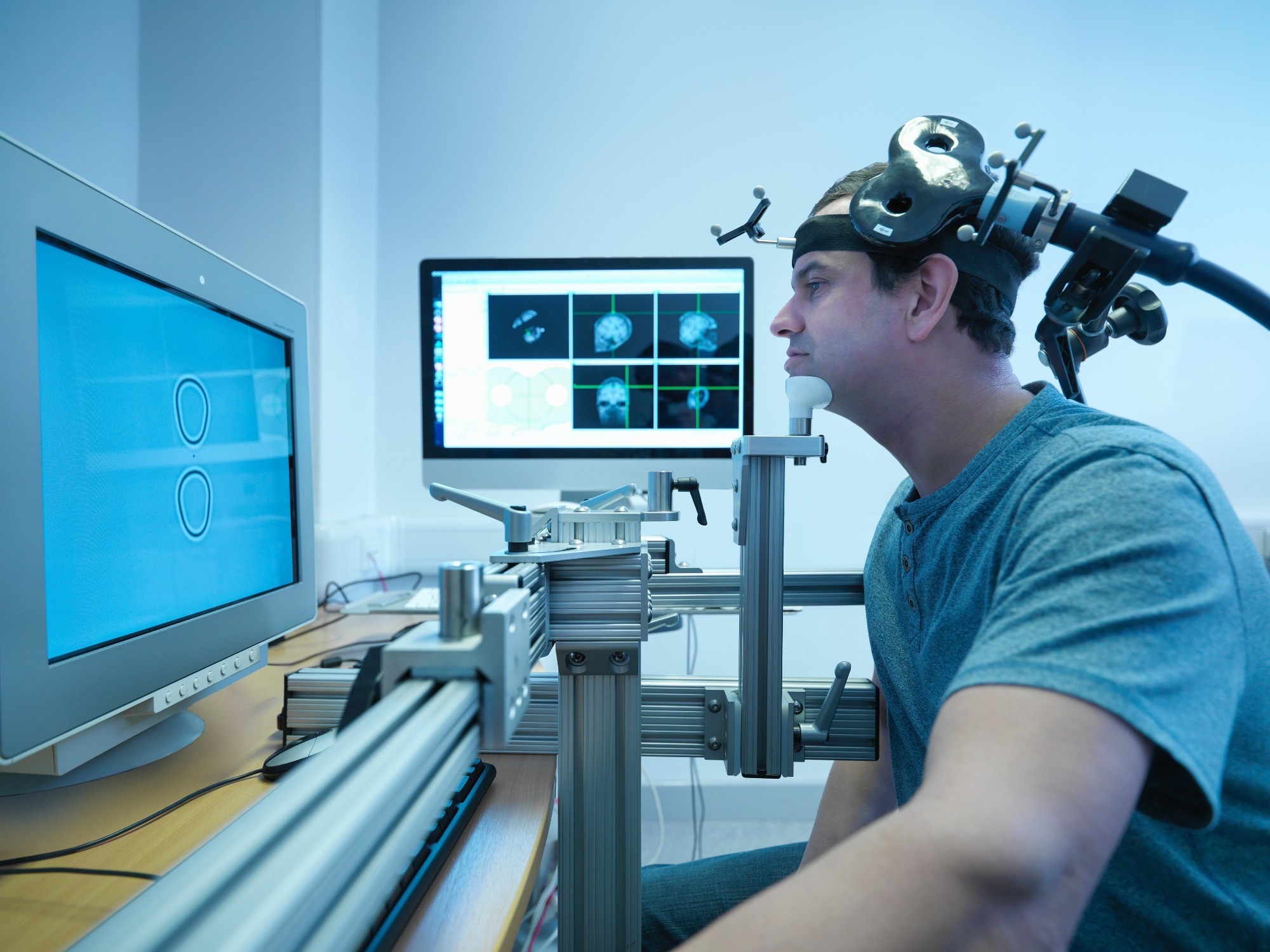
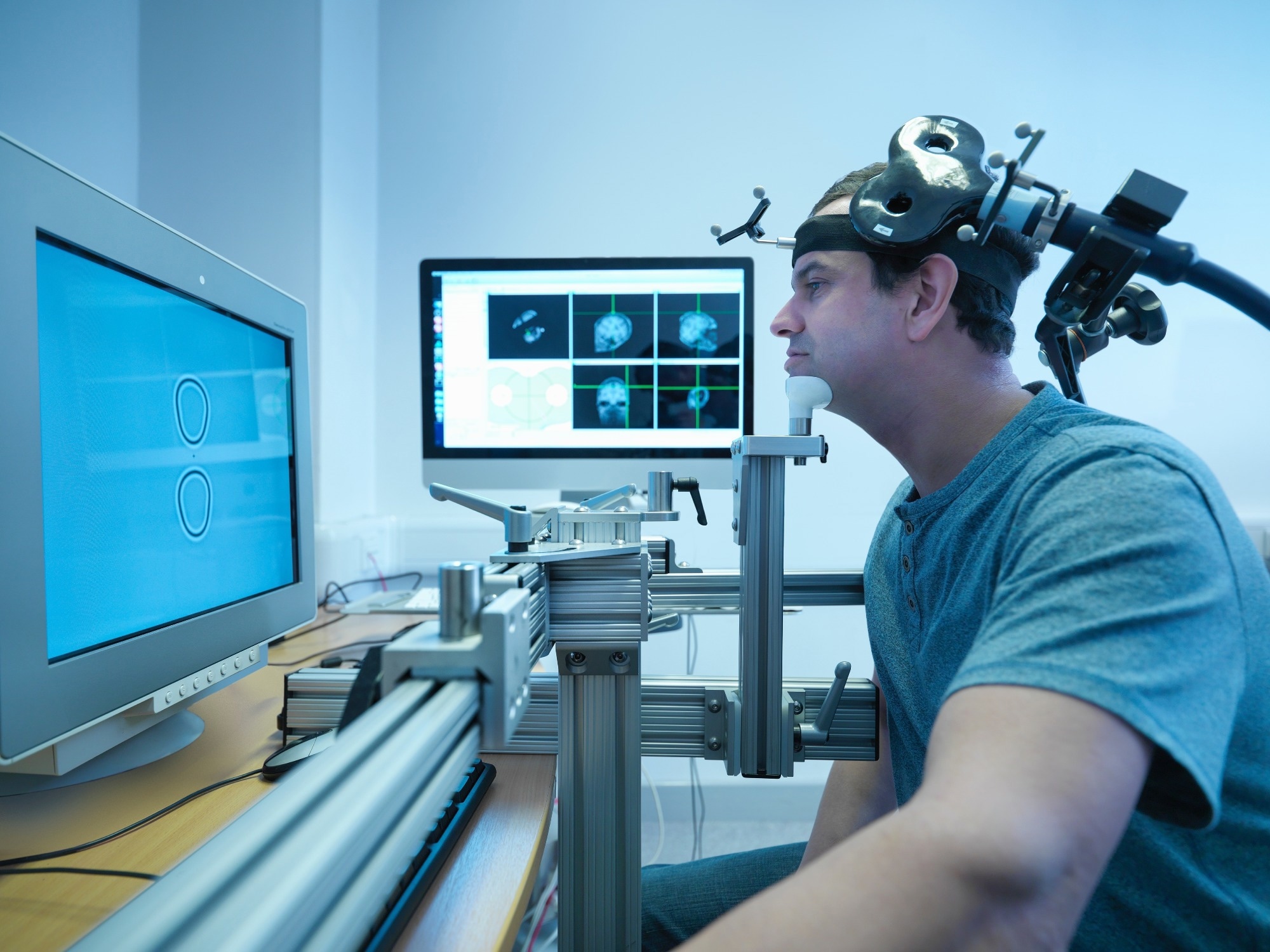
In a recent study published in the Scientific Reports, a group of researchers evaluated the efficiency, therapeutic efficacy, and patient perceptions of a custom robotic system for transcranial magnetic stimulation (TMS) coil placement in treating depression compared to traditional manual methods.
Background
TMS is a non-invasive method that uses magnetic fields to target brain neurons. Particularly in treating depression with repetitive TMS (rTMS), it is vital to focus on specific brain regions, such as the left dorsolateral prefrontal cortex (DLPFC) which exhibits reduced activity in depressed patients.
Commonly, the “5 cm rule” identifies this area, but neuronavigation provides greater accuracy. The correct coil placement is paramount for multiple reasons, including targeting, safety, consistency, customization, and optimization of stimulation parameters.
Studies have indicated that robotic TMS systems offer improved accuracy and reduced setup time compared to manual methods. Despite concerns about potential accidents with robots, research on robotic TMS’s efficacy and patient perspectives is limited.
About the study
In the present study, a positioning robot was designed for non-invasive brain stimulation to enhance the accuracy and repeatability of the stimulation process. Traditional industrial robots, due to their design, can be cumbersome when working around the human head.
In response, an innovative robotic rTMS model was created, featuring a serial arm with a spherical mechanism. This design prioritized safety and efficient movement around the brain. The advanced version of this robot had a wider workspace, larger payload, and better system stability, all tailored for stimulating the prefrontal cortex.
This robotic model retained its spherical mechanical advantages while featuring a broader workspace to accommodate an average human head size and a heavier payload for the TMS coil and its cables.
To accommodate patients of different heights, a vertically adjustable stage was added, which was set once the patient was seated and remained constant throughout the treatment. Safety mechanisms were integrated, including a braking system and a force or torque (FT) sensor, ensuring the robot stopped if unexpected events were detected.
To command the robot, an analytical solution was used, eliminating potential problems and constraining the robot’s movements. The robot’s motion was regulated at a frequency of 1 kHz, with an optical tracking system operating at 30 Hz.
Given that patients might move during the 20-minute treatment, the robot was designed to anticipate and adjust to these movements, ensuring precise coil positioning.
Using the robot in rTMS treatment offered several advantages, including more accurate and consistent robot-assisted coil placement compared to manual positioning, and enhanced treatment repeatability due to the saving of patient-specific target positions via neuronavigation.
An incorporated graphical user interface (GUI), including neuronavigation, aided in pinpointing the stimulation site using magnetic resonance imaging (MRI) data. The patient’s brain model was generated through advanced imaging techniques, allowing clinicians to target the required cortical region accurately.
Once the robot and the patient’s head positions were determined and visualized in the navigation system, the robot could move directly to the stimulation point after the initial treatment.
Further, patients diagnosed with major depressive disorder were recruited, and out of the initial fifteen, fourteen were assigned to either the robotic or manual rTMS group. The study adhered to ethical guidelines, and all participants provided informed consent.
Following preliminary evaluations, patients were assigned to receive either robotic or manual rTMS treatments over three weeks. The treatment parameters were consistent across both groups.
A set of imaging techniques, including MRI and single-photon emission computed tomography (SPECT), were used for analysis before and after treatment. The data was then statistically analyzed to determine the effectiveness and precision of both approaches.
Study results
To understand head movement during an rTMS session, researchers used a 3D measuring device to record the pose of the head. While subjects were instructed to keep their heads still, there was a gradual increase in error over time, given that their necks were not fixed in place.
The team designed two experiments comparing manual and robot-assisted adjustment methods. The first experiment evaluated the precision and speed with which the coil reached its target region in the cortical area. Findings from this experiment revealed that the manual method took almost double the time as the robot-assisted method.
This discrepancy might be even more pronounced when considering two factors: first, manual adjustments typically halted once clinicians felt they could not improve upon the current positioning error, which tended to be larger than errors seen with robotic adjustments.
Second, the robot’s speed was intentionally slowed at certain points to ensure patient safety. The study noted that the manual method generally resulted in larger errors than the robotic method. The difficulty in controlling the coil manually, as both its position and orientation need simultaneous adjustments, is a primary reason for these discrepancies.
Historical data from the team’s prior research on ultrasound stimulation placement was referenced. Compared to the TMS coil, the lighter ultrasound transducer was easier to position manually, resulting in accuracy surpassing the current experiment’s results.
The study also examined the consistency of coil placement over time. Data showed that errors in manual positioning grew significantly within just 5 minutes, leading to a shift of 9.81 mm from the original placement after 10 minutes. In contrast, the robot-assisted method showcased impressive accuracy, ending with a final position and orientation error of only 1.43 mm and 0.32°.
Regarding demographic and clinical characteristics, no significant differences were found in age, sex, or Beck Depression Inventory (BDI-II). Following the rTMS treatment, a trend toward decreased BDI scores was observed in the robot-assisted group, while the manual group showed no such change.
Notably, changes in BDI scores between the two groups were not statistically significant. SPECT analysis suggested a potential increase in rCBF in the left DLPFC for the robot-assisted group, not seen in the manual group, but the between-group differences were insignificant.
The study also utilized a questionnaire to understand potential side effects when robots are used in treatment. This questionnaire assessed comfort, setup time, repeatability, intensity, and safety during robotic rTMS.
Interestingly, despite the coil’s positioning being managed by a robot, patients reported feeling safe and comfortable. However, some reported feeling the coil was not consistently placed in the same region, even though the system was designed to maintain a consistent error margin.
The team hypothesized that patients might have unintentionally shifted the marker on their head, affecting the coil’s relative position. Another unexpected finding was that some patients felt varying stimulation intensities across sessions, which the researchers believed might be due to sensory adaptation.