The human body hosts a diverse array of microorganisms that maintain a delicate balance crucial for overall health. This microbial harmony can be disrupted by factors like infections, aging, and hormonal changes, leading to dysbiosis-;a condition where microbial communities become imbalanced and harmful to health. Postmenopausal women, for instance, are particularly susceptible to recurrent urinary tract infections and inflammation, including cystitis, due to these microbial shifts.
Dr. Takanori Sekito from the Department of Urology, Okayama University Graduate School of Medicine, Japan explains, “In postmenopausal women, the vaginal flora changes with a decrease in Lactobacillus species. Women experiencing recurrent infections of the urinary system, also known as recurrent cystitis have distinctive vaginal microbial colony compared to those with non-recurring cystitis.”
Is there a link between altered vaginal microbiota and recurrent cystitis?
Dr. Sekito teamed up with his colleagues Dr. Takuya Sadahira and Professor Motoo Araki from the Department of Urology, Okayama University Graduate School of Medicine, Japan, and Dr. Hidetada Hirakawa from the Department of Bacteriology, Gunma University Graduate School of Medicine, Japan to investigate the disease-causing bacterial colony residing in the urinary bladder and vagina of infected patients. This study, published online in Journal of Infection and Chemotherapy on June 4, 2024, highlights the association between urinary and vaginal pathogenic Escherichia coli in recurrent cystitis.
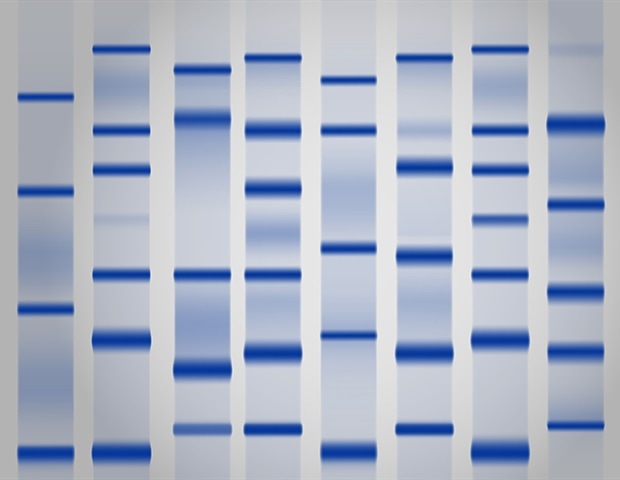
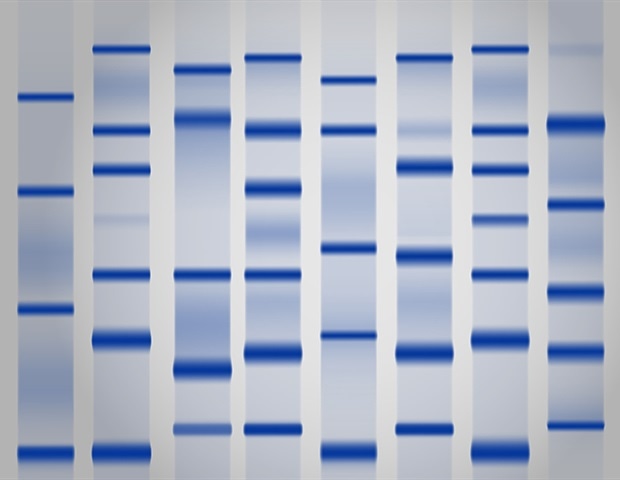
Pathogenic E. coli causes urinary tract infections. In this study, they isolated pathogenic Escherichia coli from the urine and vagina of patients with recurrent cystitis and examined the bacterial genome using multiple molecular techniques. The team also examined the sensitivity of isolated E. coli to a panel of anti-microbial agents. A dendrogram based on pulsed-field gel electrophoresis (PFGE) revealed that, in a majority of the cases, the pathogenic E. coli isolated from urine and vagina were highly similar or identical. Genomic analysis of extended-spectrum β-lactamase (ESBL) gene PCR and multilocus sequence typing (MLST) revealed that the pathogenic E. coli isolated from urine and vagina were identical. The E. coli also showed similar sensitivity to the panel of anti-microbial drugs. These findings reveal that the disease-causing pathogen was resident in both the urinary bladder and the vagina.
The authors postulate that E. coli migrates back and forth between the two niches, infecting cells in both organs and causing the disease to recur despite the prior treatment with antibiotics. Dr. Sekito explains, “The vagina can serve as a reservoir of enteric bacteria, including E. coli, and cystitis can become intractable. In recurrent cystitis, it is important to target E. coli not only in the urine but also in the vagina.”
He further, added, “At the Okayama University, we are developing Lactobacillus vaginal suppositories, as a means of prevention and treatment of recurrent cystitis. This new ‘non-antimicrobial’ prevention will reduce the unnecessary administration of antimicrobials and the consequent emergence of antimicrobial-resistant bacteria. The Lactobacillus suppositories will effectively regulate the vaginal environment and reduce the virulence of E. coli.”
In summary, this study highlights the crucial need to balance the microbial environment to favor protective bacteria for better health outcomes. Implementing new medical strategies based on these insights promises to revolutionize the management of recurrent cystitis, ensuring more effective and targeted treatments.
Source:
Journal reference:
Sekito, T., et al. (2024). Homology of Escherichia coli isolated from urine and vagina and their antimicrobial susceptibility in postmenopausal women with recurrent cystitis. Journal of Infection and Chemotherapy. doi.org/10.1016/j.jiac.2024.05.015.