The tendency of the body’s immune system to selectively use immunological memory, based on a past infection whenever a variant of a pathogen (for example – a virus or bacteria) is encountered, is referred to as ‘antigenic imprinting’.
Group 1 influenza A viruses are H1N1 and H2N2, and group 2 influenza A virus is H3N2. Previously, differential vulnerability to other potentially lethal influenza viruses, such as H5N1 and H7N9, has been linked to an individual’s first viral subtype exposure to influenza A virus at a younger age.
Imprints of this kind can have long-lasting impacts on antigen-specific protection, which can be favorable, neutral, or negative. Knowledge about this phenomenon will likely aid in evaluating and strategizing better vaccination protocols against a particular target.
Background
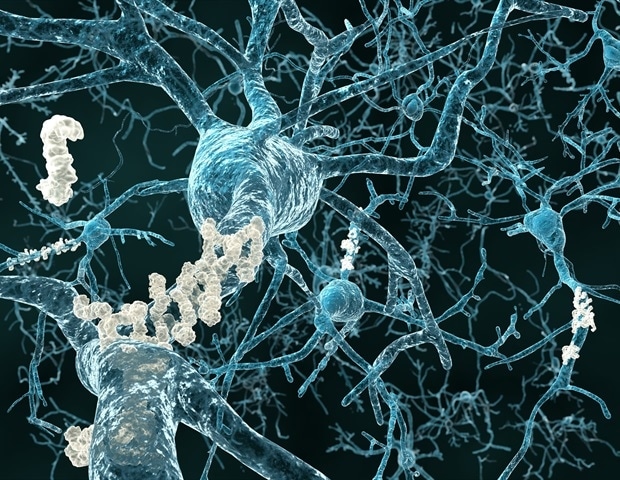
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at the end of 2019 has precipitated the ongoing global pandemic. It is now known that previous seasonal coronavirus infections inhibit the development of immunoglobin G (IgG) and IgM against SARS-CoV-2, suggesting immunological imprinting from other beta coronaviruses. Yet, the potential range, effects, and processes of antigenic imprinting in exposure to multiple SARS-CoV-2 variants are only beginning to be uncovered.
The Omicron strain is a rapidly disseminating and immuno-evasive variant of concern (VOC) of SARS-CoV-2. This mutant can breach the protective immunity gained through COVID-19 vaccines and evade most monoclonal antibody (mAb) treatments.
Previous investigations have shown that three doses of the ancestral messenger ribonucleic acid (mRNA) vaccine confers neutralization titers against the Omicron variant, comparable to the levels effective for Delta neutralization, after two mRNA vaccinations.
Of note, Omicron emergence had initially prompted the development of mRNA vaccines based on the Omicron sequence to facilitate additional benefits when administered as a booster or as a primary vaccination dose. However, a significant difference could not be observed in macaque trials––that compared the booster doses with an ancestral wild-type mRNA vaccine targeting the Omicron or Beta mRNA vaccines––concerning the neutralization titer or disease protection.
The first human trials using a Beta- or Delta-based mRNA booster vaccine dose elicited equivalent neutralization titers with multiple variant booster administrations.
On the other hand, nonimmunized individuals who contracted an infection with either the Alpha or Delta variant had antibodies that showed preferential binding to the receptor-binding domain (RBD) of the corresponding strain. Individuals who had been immunized against the ancestral strain and experienced breakthroughs with the Alpha or Delta strains exhibited RBD-binding patterns identical to the non-immunized individuals convalescent with the ancestral strain only.
The study and findings
A recently published study in Clinical and Translational Medicine compared monoclonal RBD antibody responses induced by SARS-CoV-2 Beta variant infections to antibodies induced by the ancestral virus in immunologically naive subjects. It was observed that most Beta-elicited mAbs – isolated from memory B cells, did not bind the ancestral strain, whereas others potently neutralized the Beta, the ancestral strain, and other VOCs. Thus, immunization with an antigenically distant SARS-CoV-2 mutant can trigger variant-specific memory B cells that establish a distinct imprint for which memory B cells are available for subsequent recall with the same or variant antigen.
The functional relevance of antigenic imprinting in SARS-CoV-2 immunity against variants and its possible implications for (booster) vaccination methods are crucial in analyzing the mAbs elicited in individuals exposed to multiple viral variants (s).
Furthermore, research findings examining the antibody response to Omicron outbreaks were (pre)published. The findings depicted that Omicron infections increase the rate of pre-existing memory B cells that recognize conserved epitopes instead of evoking new B cells against Omicron-specific epitopes. This observation emphasized the significance of antigenic imprinting in SARS-CoV-2. Here, the neutralizing activity of convalescent serum was enhanced not only against Omicron but also against prior SARS-CoV-2 VOCs and severe acute respiratory syndrome coronavirus (SARS-CoV).
Other reports suggested that antibodies preferred recognizing and neutralizing the original SARS-CoV-2 strain in the initial stages, suggesting that vaccine-induced memory B cells were activated early on.
Hence, Omicron breakthrough infections preferentially activate cross-reactive memory B cells; antigenic imprinting is critical in deciding SARS-CoV-2 immunity to viral variations.
Furthermore, antigenic imprinting from parental strain mRNA vaccines does not affect the immune response towards Omicron, and so there are currently no imprint-related concerns about the effectiveness of current immunization techniques.
Nonetheless, ambiguity remains. Future longitudinal studies will help in the understanding of the concept of SARS-CoV-2 B-cell recall and record single antibody clones and their variant-specific maturation.
Additionally, owing to the unpredictability of the upcoming mutations, the function of antigenic imprinting in SARS-CoV-2 immunity may alter rapidly and substantially in the future, and the overall effects could be favorable or harmful. Therefore, the influence of immunological imprinting should be closely observed when newer emerging viral mutants are evaluated to gauge its ramifications and to alter vaccination strategies.