An article published in the journal PNAS provides a conceptual analysis to interpret the brain state of coronavirus disease 2019 (COVID-19) patients experiencing prolonged recovery of consciousness.
 Study: Protective down-regulated states in the human brain: A possible lesson from COVID-19. Image Credit: Jay Ondreicka / Shutterstock
Study: Protective down-regulated states in the human brain: A possible lesson from COVID-19. Image Credit: Jay Ondreicka / Shutterstock
Background
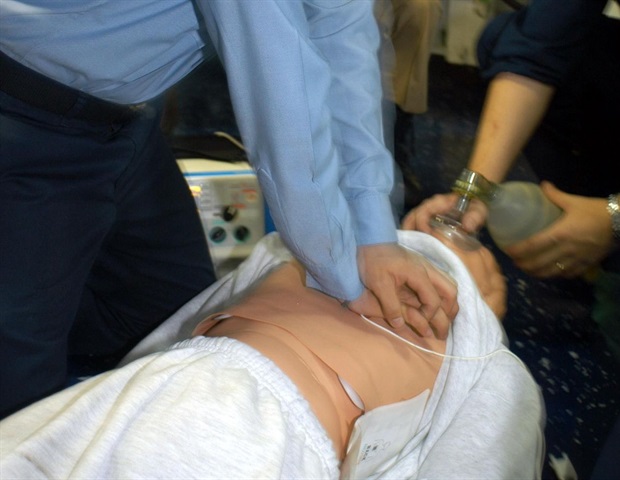
Prolonged mechanical ventilation with multiple anesthetics is commonly used to treat critically ill COVID-19 patients in intensive care units.
These patients exhibit a very slow recovery of consciousness following the treatment. This could be due to post-operative neurocognitive disorders induced by anesthetics. Another important causal factor is severe hypoxia associated with acute respiratory distress syndrome in COVID-19 patients. However, no change in brain structure is usually observed in these patients.
Burst suppression is a brain electrical pattern characterized by a cycling of suppressed cerebral activity and bursts of cerebral activity of variable amplitude, duration, and waveform. It is considered to be a sign of neuroprotective activity. Severe COVID-19 patients exhibit comparable burst suppression to those experiencing prolonged unconsciousness following cardiac arrest.
Burst suppression is commonly associated with hypoxic brain injury, low brain temperature, high-dose anesthetics, cortical abnormalities, and severe seizures. All these conditions are associated with a hypoxia-related reduction in brain metabolic activity.
Hypoxia-induced suppression of neuronal activity as a neuroprotective mechanism
The Ching model is a biophysically based mathematical model to study burst suppression. This model has been used to study cognitive recovery in post-cardiac arrest coma patients treated with hypothermia.
Electroencephalography (EEG) of the patients shows burst suppression. All of them eventually experience full cognitive and physical recovery. As mentioned by the scientists, burst suppression characterized by reduced brain metabolism plays an essential neuroprotective role in these patients.
Trace alternant is a neonatal sleep pattern that reflects an energy conservation state. The EEG pattern of trace alternant is significantly associated with burst suppression EEG pattern. Both phenomena reflect a vital approach for preserving neural integrity through the downregulation of brain energy metabolism.
The EEG pattern observed in a painted turtle, an anoxia-resistant vertebrate, is almost identical to the trace alternant EEG pattern. During the winter, this turtle experiences severe anoxic conditions and exhibits a marked temperature-dependent neuroprotective response.
The anoxic exposure increases the release of a neurotransmitter (GABA), which in turn causes a downregulation in neuronal and metabolic activities in the turtle brain. This highlights the link between anoxic exposure and the establishment of a neuroprotective state.
In COVID-19 patients, severe hypoxia is known to cause neuronal injury. In addition, hypoxic brain injury is also associated with the downregulation of metabolic activity. Collectively, these processes can alter the state of consciousness of a patient.
Despite the possibility of hypoxia-induced neuronal injury, the prolonged recovery of consciousness observed in COVID-19 patients after mechanical ventilation indicates the protective effects of reduced neuronal activity. This event is similar to that observed in patients recovering from post-cardiac arrest coma and in anoxia-resistant turtles.
Prolonged unconsciousness following severe COVID-19 as a neuroprotective mechanism
Anoxia-resistant turtles exhibit a protective downregulated brain state that helps reduce the brain energy demand during systemic metabolic stress caused by anoxia or extreme temperature. Such protective mechanisms might also be present in the human brain.
In this context, scientists have hypothesized that hypoxia, along with specific therapeutics (GABAergic anesthetics and hypothermia), might induce similar protective mechanisms through global suppression of brain metabolism in human, which result in prolonged recovery of consciousness in severe COVID-19 patients after mechanical ventilation or in post-cardiac arrest coma patients.
Management of prolonged recovery of consciousness in COVID-19 patients
In anoxia-resistant animals, the brain energy level should be maintained following anoxia exposure to prevent neuronal death. In COVID-19 patients, hypoxia and inflammation are expected to cause mitochondrial dysfunction. Thus, therapeutic interventions to stimulate mitochondrial energy production may benefit severe COVID-19 patients experiencing prolonged recovery of consciousness after mechanical ventilation.
Szeto-Schiller peptides are currently under clinical investigation for their ability to rapidly restore mitochondrial energy levels in aged rodents to that of young rodents. These peptides work by increasing mitochondrial ATP production, which in turn helps mitigate post-hypoxic neuronal injury (ATP therapy).
Severe COVID-19 patients could be treated with a combination of direct ATP therapy and pharmacological agents used to treat cognitive impairment. In this context, amantadine, the first-line glutamatergic drug for treating consciousness disorders, could be used combined with donepezil, a cholinergic agonist, as an effective strategy to overcome post-COVID neurological deficits.


%2c_3D_illustration._A_virus_transmitted_by_mosquito_and_caus_-_Kateryna_Kon_M1_cd7c644c9e204869b1de65dd2f361793-620x480.jpg)


