In a recent study published in the journal Psychiatry Research, a group of researchers evaluated the effects of a ketogenic diet (KD) on metabolic and psychiatric health in individuals with schizophrenia or bipolar disorder with existing metabolic abnormalities.
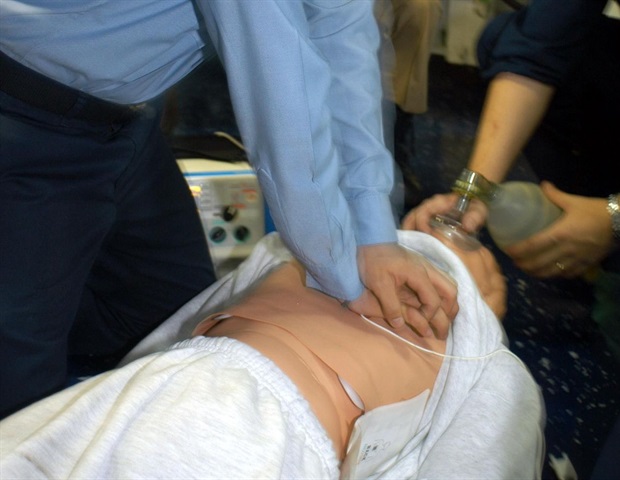
 Study: Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Image Credit: Maglara / Shutterstock
Study: Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Image Credit: Maglara / Shutterstock
Background
Millions worldwide suffer from severe mental illnesses, such as schizophrenia (24 million) and bipolar disorder (50 million). Current treatments often lead to resistance or metabolic side effects, causing nonadherence. Traditional neuroleptics can reduce life expectancy despite benefiting long-term mortality in schizophrenia. The KD, effective in treating epilepsy, offers an alternative fuel source for the brain, reducing neuronal excitability and inflammation. Emerging evidence suggests metabolic dysfunction underpins psychiatric diseases. Given the high risk of metabolic syndrome in those with severe mental illness, further research on KD’s potential to improve metabolic and psychiatric outcomes is crucial.
About the study
The present study involved 23 participants aged 18-75, all on psychotropic medications and meeting the criteria for being overweight or having a metabolic abnormality. Twenty-one participants completed the trial (5 with schizophrenia and 16 with bipolar disorder). Eligibility was determined through comprehensive assessments and laboratory tests. Participants received educational materials, cookbooks, resources, and a personal coach.
The KD prescribed consisted of 10% carbohydrates, 30% protein, and 60% fat, aiming for blood ketone levels between 0.5-5 mM. Compliance was monitored based on ketosis levels. Blood samples were analyzed for metabolic markers, and vital signs, body composition, and psychiatric evaluations were recorded at baseline, two months, and four months. Remote participants self-reported data and attended local facilities for assessments. The study also evaluated the potential side effects of the KD compared to psychiatric medications and was approved by the Stanford University Institutional Review Board and registered with ClinicalTrials.gov (NCT03935854).
Statistical analyses were performed using standard methods in Microsoft Excel, with data recorded in Research Electronic Data Capture (REdCap). Paired t-tests compared baseline and final measurements, and McNemar’s Test and Chi-squared analysis assessed nominal data. The study, exploratory in nature, was not powered for significance, but p-values <0.05 were considered significant. The analysis included percent changes in metabolic and psychiatric outcomes, providing insights into the KD’s potential benefits for individuals with severe mental illnesses.
Study results
The data analysis cohort included twenty-three participants, comprising 5 with schizophrenia and 16 with bipolar disorder. Fourteen participants were fully adherent to the KD, six were semi-adherent, and one was non-adherent.
Initially, 29% of participants met the criteria for metabolic syndrome. By the end of the study, none met these criteria (p < 0.05). Key metabolic outcomes included a 10% average weight reduction (p < 0.001), an 11% reduction in waist circumference (p < 0.001), a 6.4% decrease in systolic blood pressure (p < 0.005), a 17% reduction in fat mass index (p < 0.001), and a 10% reduction in body mass index (BMI) (p < 0.001). Visceral adipose tissue decreased by 27% (p < 0.001), high–sensitivity reactive protein (hsCRP) by 23%, triglycerides by 20% (p < 0.02), and small dense low–density lipoprotein (LDL) by 1.3%. Increases were observed in LDL (21%) and high–density lipoprotein (HDL) (2.7%). Hemoglobin A1c (HbA1c) decreased by 3.6% (p < 0.001), and Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) by 17% (p < 0.05). There was no significant change in the 10-year Atherosclerotic Cardiovascular Disease (ASCVD) risk score for the whole cohort, but adherent participants showed an 11% improvement (p < 0.01).
Psychiatric outcomes revealed a 31% improvement in Clinical Global Impressions severity scores (p < 0.001). Recovery rates increased from 33% at baseline to 75% by study end, with 100% recovery in the adherent group. Overall, 43% of participants achieved recovery (50% adherent, 33% semi-adherent), with 79% showing marked improvement in severity (92% adherent, 50% semi-adherent). Among bipolar participants, 69% showed >1 point improvement in severity, with recovery rates increasing from 38% to 81%. All adherent bipolar participants were in recovery or recovering by the study’s end. Psychiatric improvements included a 17% increase in life satisfaction (p < 0.002), a 17% improvement in Global Assessment of Functioning (p < 0.001), and a 19% improvement in sleep quality (p < 0.02). Schizophrenia participants experienced a 32% reduction in Brief Psychiatric Rating Scale scores (p < 0.02).
Common side effects of the KD, such as headache, fatigue, and constipation, were initially documented but diminished to minimal levels after the third week. Participants’ qualitative feedback highlighted significant improvements in anxiety, mood stabilization, and overall life quality, with some expressing profound personal transformations.
Conclusions
To summarize, the study on individuals with schizophrenia and bipolar disorder undergoing a KD alongside psychiatric medication revealed significant psychiatric and metabolic improvements. Psychiatric outcomes showed a 31% improvement in mental illness severity, with 79% of symptomatic participants experiencing meaningful improvement, particularly among adherents. Metabolic outcomes included reductions in weight, waist circumference, systolic blood pressure, fat mass index, BMI, visceral adipose tissue, HbA1c, and triglycerides. Common KD side effects diminished after three weeks. These findings suggest that KD is a feasible and effective supplemental treatment, improving this population’s psychiatric and metabolic health.