Research highlights how microbial imbalances elevate susceptibility to infection and reinfection, offering potential pathways for prevention and treatment.
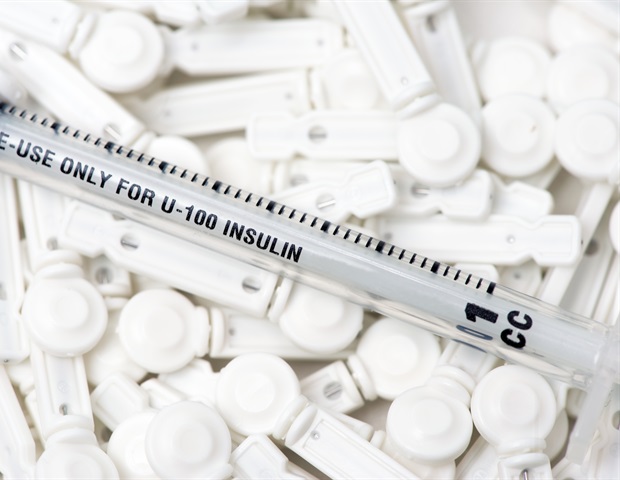
 Study: Cervicovaginal microbiome and natural history of Chlamydia trachomatis in adolescents and young women. Image Credit: Arif biswas/Shutterstock.com
Study: Cervicovaginal microbiome and natural history of Chlamydia trachomatis in adolescents and young women. Image Credit: Arif biswas/Shutterstock.com
The cervicovaginal microbiome (CVM) plays a crucial role in influencing the risk of genital tract infections. A recent study published in Cell examines how the CVM impacts the incidence and recurrence of Chlamydia trachomatis (CT) infections and their associated complications.
Understanding Chlamydia trachomatis
CT is the most common bacterial sexually transmitted infection (STI), with over 130 million cases reported in 2019. Its rising incidence over the past four decades has placed a significant burden on public health systems.
CT can lead to serious complications, including pelvic inflammatory disease (PID), miscarriage, chronic pelvic pain, infertility, and ectopic pregnancy. Infants born to mothers with CT are at risk for conjunctivitis and pneumonitis.
Adolescents and young adults (AYA) account for half of all new STI cases, with CT rates five times higher among Black and Hispanic AYAs compared to their White counterparts, highlighting stark disparities in health outcomes. Risk factors for CT include multiple sexual partners, previous STIs, age under 25, low educational attainment, and vaginal dysbiosis, commonly referred to as bacterial vaginosis (BV). However, since BV and CT share similar risk factors, their relationship remains complex and disentangled.
The cervicovaginal microbiome
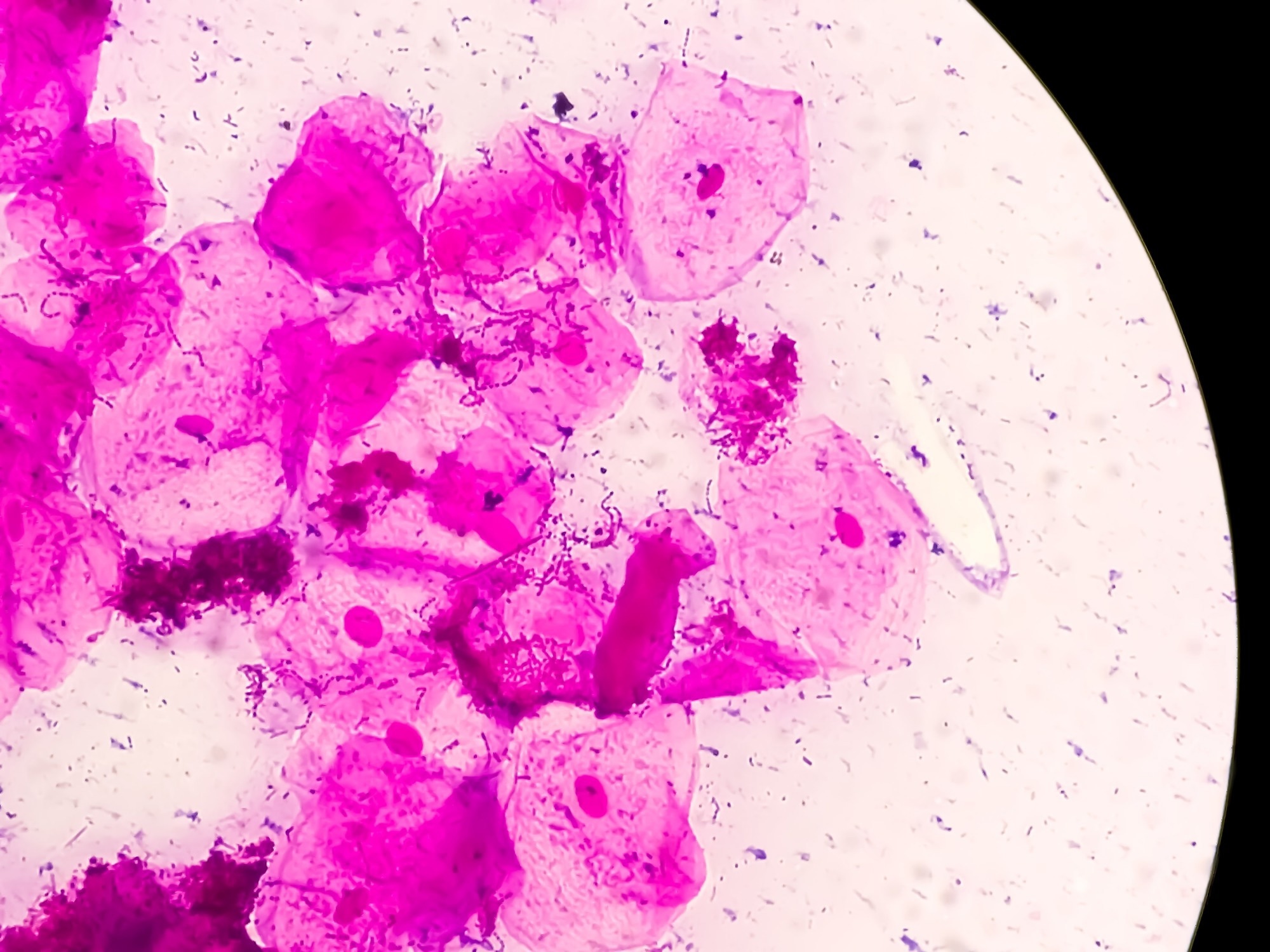
The CVM consists of bacteria and fungi, typically dominated by lactobacilli or characterized as polymicrobial. Key lactobacillus species—L. crispatus, L. iners, L. gasseri, and L. jensenii—produce lactic acid, creating an environment that inhibits CT colonization. Some species also reduce tryptophan levels, further limiting CT growth.
The CVM is categorized into molecular subtypes based on 16S rRNA gene sequencing and community state type (CST) clustering.
Study overview
The study aimed to explore the link between BV and CT over time while controlling for shared risk factors. Researchers examined 560 Black and Hispanic AYAs, including 187 women with newly diagnosed CT infections and 373 controls. Participants aged 13 to 21 years (mean age 20) were all sexually active.
CVM samples were collected approximately six months before infection, during infection, and six months post-infection. These samples were analyzed using a molecular BV score (molBV), an objective marker of CVM status, similar to the Nugent score used to diagnose BV.
Predicting CT risk
MolBV scores were significantly higher among individuals who later developed CT compared to controls. This difference was evident in pre-infection samples but disappeared after treatment, suggesting CVM dysbiosis may increase susceptibility to CT.
Participants with BV-like CVM features, characterized by higher molBV scores and greater microbial diversity, showed a higher risk of CT. Specifically, CST-IV-A, a subtype associated with Candidatus Lachnocurva vaginae, increased CT risk by 2.5 times and was linked to recurrent infections.
Further stratification revealed that individuals with an mBV-positive CVM profile were 62% more likely to acquire CT. Those classified as mBV-A (associated with CST-IV-A) had a 2.4-fold higher risk compared to mBV-B.
Candidatus Lachnocurva vaginae—33 times more prevalent in mBV-A—may disrupt protective lactic acid production, weakening the defense against CT. This species was closely linked to a network of ten bacterial genera, including Prevotella, Megasphaera, and Clostridium, which collectively predicted a 2.5-fold increase in CT risk per unit rise in microbial risk score (MRS).
Broader impacts on the CVM
CT infections caused significant changes in the CVM, although post-treatment samples often returned to baseline composition. However, mBV-intermediate states and CST-IV-A remained elevated in CT cases compared to controls.
The mBV-A state not only predicted new infections but also increased reinfection risk by 3.6 times. Overall, reinfection rates were 20.6% among CT cases versus 4% in controls, representing a sixfold higher risk.
Additionally, the mBV-positive state post-treatment correlated with increased rates of miscarriage, underscoring the clinical significance of CVM composition.
Conclusions
The study concludes that CVM features associated with BV—such as mBV states, CSTs, and specific bacterial taxa—strongly predict the risk of CT infection and reinfection. The loss of protective lactobacilli and increased microbial diversity provide biological support for these findings.
These results highlight the importance of classifying BV by molecular subtype to understand its relationship with CT better. The CVM’s role in susceptibility, recurrence, and complications also underscores its potential as a target for preventive and therapeutic interventions.