A recent study published in the New England Journal of Medicine evaluated the burden and risk of post-acute sequelae of coronavirus disease 2019 (COVID-19) (PASC) during the pre-Delta, Delta, and Omicron periods.
PASC, also known as long COVID, affects several organ systems. Its risk increases with the severity of infection and preexisting conditions but decreases after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination. Although PASC has been reported with distinct SARS-CoV-2 variants, it is speculated that variations in viral characteristics, among other factors, may have reduced PASC risk. However, whether PASC risk was altered and to what extent remains unclear.
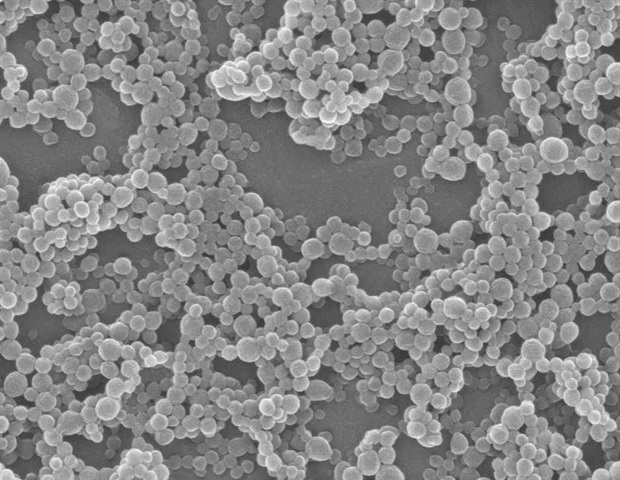
 Study: Postacute Sequelae of SARS-CoV-2 Infection in the Pre-Delta, Delta, and Omicron Eras. Image Credit: p.ill.i / Shutterstock
Study: Postacute Sequelae of SARS-CoV-2 Infection in the Pre-Delta, Delta, and Omicron Eras. Image Credit: p.ill.i / Shutterstock
About the study
In the present study, researchers compared PASC risk and burden during the pre-Delta, Delta, and Omicron waves of the COVID-19 pandemic. They selected veterans with COVID-19 between March 2020 and January 2022. They were stratified into five cohorts: non-vaccinated and infected during 1) pre-Delta, 2) Delta, and 3) Omicron waves, and vaccinated and infected during 4) Delta and 5) Omicron waves.
In addition, three wave-specific control cohorts included SARS-CoV-2 infection-naïve individuals. COVID-19 cohorts were followed up from infection until one year, reinfection, or death. Controls were followed up until the first SARS-CoV-2 infection, one year, or death. The researchers examined prespecified health outcomes, stratified into ten categories – fatigue, cardiovascular, gastrointestinal, mental health, pulmonary, neurologic, musculoskeletal, metabolic, kidney, and coagulation and hematologic.
An incident outcome was defined as one that occurred between 30 days and 12 months post-infection. Further, the number of disability-adjusted life years due to PASC was estimated. Data on covariates were obtained before baseline. Differences in baseline characteristics among cohorts were assessed. The cumulative incidence of PASC was estimated using weighted generalized estimating equations with Poisson regression.
PASC risk and burden were evaluated based on the difference(s) in these measures between COVID-19 and control cohorts. These measures were compared among COVID-19 cohorts and evaluated in combined COVID-19 cohorts. Decomposition analyses examined the contribution of vaccines and eras to changes in PASC incidence. Several sensitivity analyses were also performed.
Findings
The COVID-19 cohorts included 441,583 veterans, and the control cohorts comprised over 4.74 million individuals. The cumulative PASC incidence a year post-infection was 10.42, 9.51, and 7.76 events per 100 individuals among non-vaccinated cohorts during the pre-Delta, Delta, and Omicron periods, respectively. It was lower during the Omicron period than during pre-Delta and Delta waves.
In vaccinated cohorts, the cumulative PASC incidence was 5.34 and 3.5 events per 100 individuals during the Delta and Omicron waves, respectively. It was lower among vaccinated subjects compared to non-vaccinated individuals. By disease category, the risk of sequelae was lower for most categories, albeit higher for musculoskeletal, gastrointestinal, and metabolic disorders during the Omicron period.
Decomposition analyses indicated 5.23 fewer PASC events during the Omicron period than during the other two periods combined, representing a 51.77% decline. A vast proportion (71.8%) of this decline was attributed to vaccines, while era-related effects accounted for over 28%. Sensitivity analyses yielded consistent findings.
Conclusions
The cumulative PASC incidence decreased throughout the COVID-19 pandemic, from 10.42 cases in the pre-Delta period to 3.5 cases during the Omicron era. Nevertheless, it was not negligible during the Omicron era. Notably, the sample predominantly included older White males and, thus, might not be representative of the general population. The study’s observational nature is subject to biases, such as misclassification bias and residual confounding.
Further, the findings reflect PASC risk among those who were SARS-CoV-2-positive relative to infection-naïve controls. As such, individuals with undiagnosed infection may have asymptomatic or mild disease and differential PASC risks. Together, the study revealed the contributions of vaccinations and temporal effects to reducing the PASC burden over the pandemic, albeit substantial residual risk still prevails among vaccinated subjects infected in the Omicron era.
@NEJM Major #LongCovid report by @zalaly @Biostayan @WUSTLmed
Good news: The rate is dropping with vaccination and infection-induced immunity
Bad news: It’s still affecting 3.5% of people who get Covid, significant disabilityhttps://t.co/sBOLoV4Bf1 pic.twitter.com/AGZFhwgzes— Eric Topol (@EricTopol) July 17, 2024