The gut microbiome plays an active role in maintaining an individual’s health. Alteration in the gut microbial population (dysbiosis) can influence disease severity and impact long-term outcomes in adults infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Owing to limited sample availability, the impact of the gut microbiome in children with COVID-19 has not been evaluated.
One of the reasons for lower sample availability is that children are at lower risk of contracting SARS-CoV-2 compared to adults.
Recently, scientists have reviewed the available evidence on the gut microbiome in children with COVID-19 and published it in Microorganisms.
Background
Most children with COVID-19 experience at least one gastrointestinal (GI) infection symptom, such as abdominal pain, vomiting, and diarrhea. All these symptoms are linked with changes in the patient’s gut microbiome.
Not much data is available on the prevalence of asymptomatic children with COVID-19. Nevertheless, the stool analysis of asymptomatic infants with COVID-19 revealed a decrease in Enterocloster clostridioformis, Bifidobacterium bifidum, Akkermansia muciniphila, and Veillonella dispar. In adults, gut microbiome dysbiosis has been correlated with higher levels of inflammatory cytokines in patients severely infected with SARS-CoV-2.
In different gestational stages of pregnancy, the gut microbiome promotes various inflammatory responses. Multiple prenatal and early life factors, which include SARS-CoV-2 infection during pregnancy, influence the development of the gut microbiome in infants. Breast milk also plays an important role in infants’ development of a healthy gut microbiome.
As the risk of transmission of SARS-CoV-2 from mother to infant through breast milk is low, it has been recommended that infants should continue to receive breast milk from mothers with SARS-CoV-2 infection, following the safety guidelines.
Although most children remain asymptomatic or experience mild symptoms after SARS-CoV-2 infection, some develop multisystem inflammatory syndrome in children (MIS-C), which is a severe condition. Since GI symptoms are prominent MIS-C symptoms, it has been conjectured that the gut microbiome might act as local and systematic inflammatory modulators via interactions with SARS-CoV-2.
A significant difference in beta diversity was found between MIS-C and healthy children. Even though not much research is available on the role of the gut microbiota in the pathogenesis of MIS-C, a decrease in the anti-inflammatory taxa and an elevation of pro-inflammatory taxa has been observed. Furthermore, comorbidities, such as type 2 diabetes, obesity, and high blood pressure, have been associated with gut microbiome imbalance. This imbalance promotes inflammatory dysfunctions that worsen COVID-19 symptoms.
Underlying mechanisms
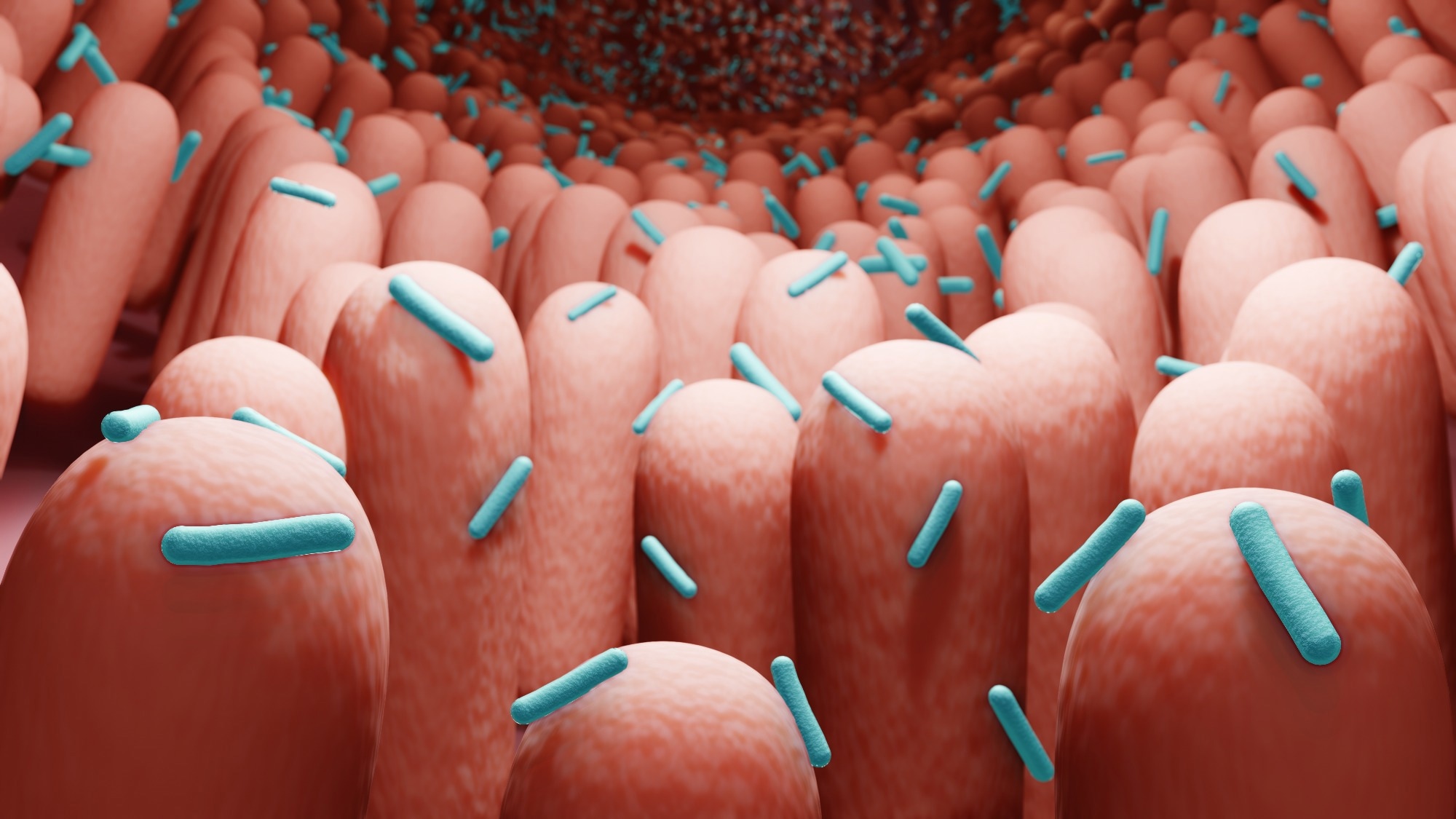
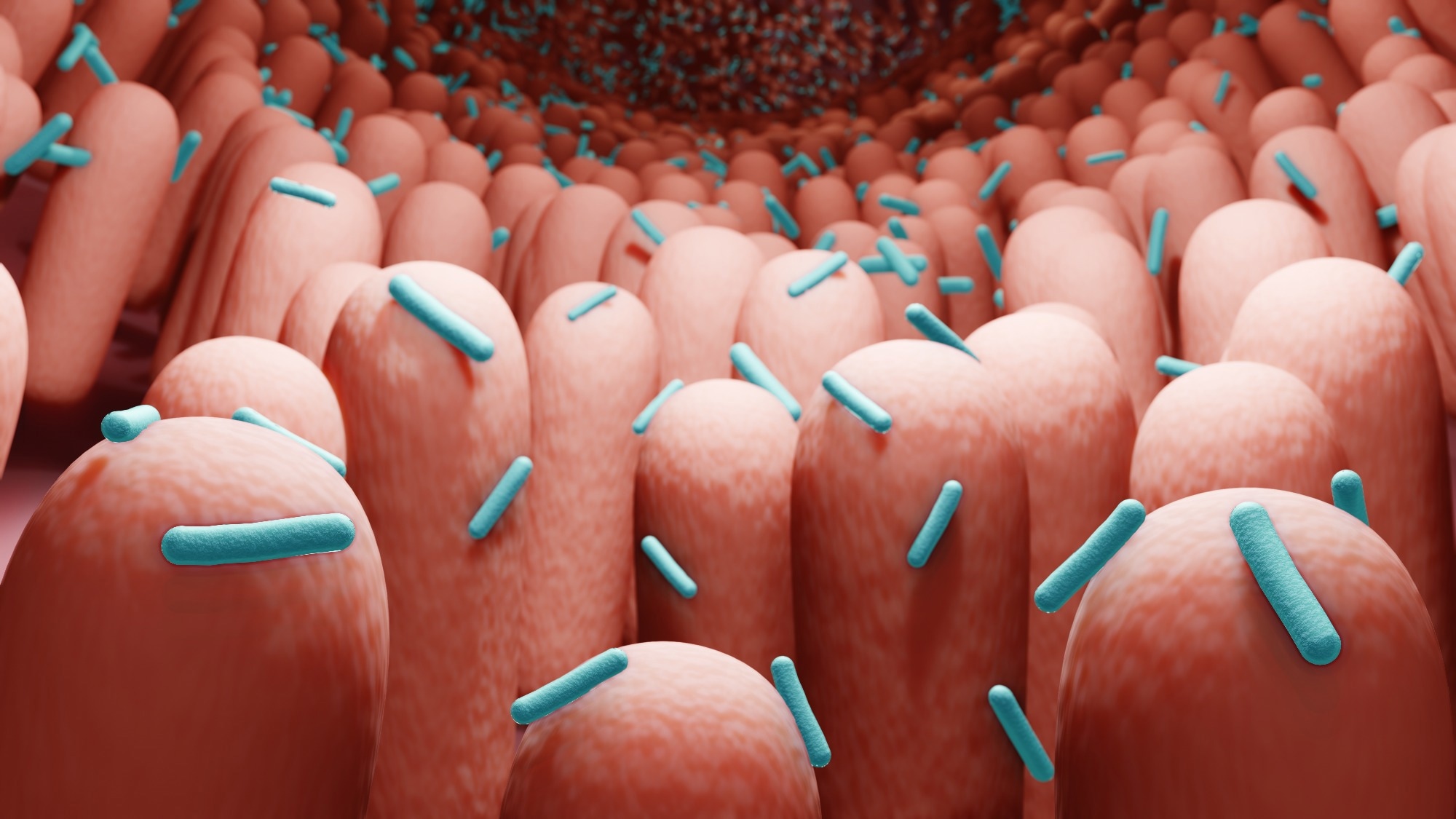
The gut microbiome in children differs from adults. It is extremely important to understand the mechanisms associated with the interactions between gut microbiota and SARS-CoV-2. Scientists identified possible mechanisms of the gut microbiome, such as gut barrier integrity, the immune system, ACE2 receptor expression, and difference in microbiota composition and metabolites, which significantly contribute to clinical outcomes in children and adults.
The change in the gut microbial composition throughout one’s life influences the shaping of the immune and metabolic systems. Children’s gut microbiome comprises an abundance of taxa from Bacteroidetes and Actinobacteria. Notably, gut microbiota composition correlates with disease severity and levels of inflammatory markers and cytokine concentration in adult COVID-19 patients. Children with mild COVID-19 symptoms showed a high prevalence of Actinobacteria and Firmicutes, while Bacteroidetes and Proteobacteria were found in those with severe infection.
Intestinal inflammation, gut barrier dysfunction, and microbial translocation also cause alterations in the gut microbiome. The presence of SARS-CoV-2 in the GI tract causes a release of zonulin, a regulator of tight intercellular junctions between epithelial cells. The high level of zonulin elevates intestinal permeability. Increased gut permeability promotes the trafficking of SARS-CoV-2 antigens into the bloodstream, which leads to hyperinflammation. In addition, enhanced gut permeability causes microbial translocation in the gut.
Microbial therapeutics for children with COVID-19
The gut microbiome is important in establishing vaccine immune response and efficacy. Specific gut bacterial taxa have been associated with higher immune response post mRNA-based COVID-19 vaccination. For example, higher Bifidobacterium adolescentis were correlated with a higher concentration of neutralizing antibodies for the inactivated COVID-19 vaccine.
Microbial therapeutics that include probiotics, prebiotics, synbiotics, and fecal microbiota transplantation (FMT), support the development of a healthy gut microbiome. Oral microbial therapeutics have been used in children to prevent or reduce the severity of respiratory infections. This treatment demonstrated significant antiviral effects by regulating the host inflammatory response and strengthening their gut–lung axis.
In obese adults, daily probiotics were found to substantially reduce upper respiratory tract infection symptoms and stabilize gut microbiota diversity. This is relevant and desirable for COVID-19 infection, as obesity causes unwanted outcomes. Also, probiotic treatment reduced hospitalization time and decreased IL-6 levels. In the future, more research is required to determine the efficacy of oral microbial therapeutics in treating SARS-CoV-2 infection in pediatric populations.