Clinical presentation following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) ranges from mild self-limiting illness to severe respiratory failure. Many studies have analyzed the early acute phases of coronavirus disease 2019(COVID-19), but few focused on the longer-term sequelae following infection. Although most affected individuals recover fully, a significant proportion suffers long-term health consequences. These individuals experience a wide range of symptoms, termed the post–COVID-19 syndrome. In addition, pulmonary function impairment occurs in some affected individuals; however, its mechanism is still unclear.
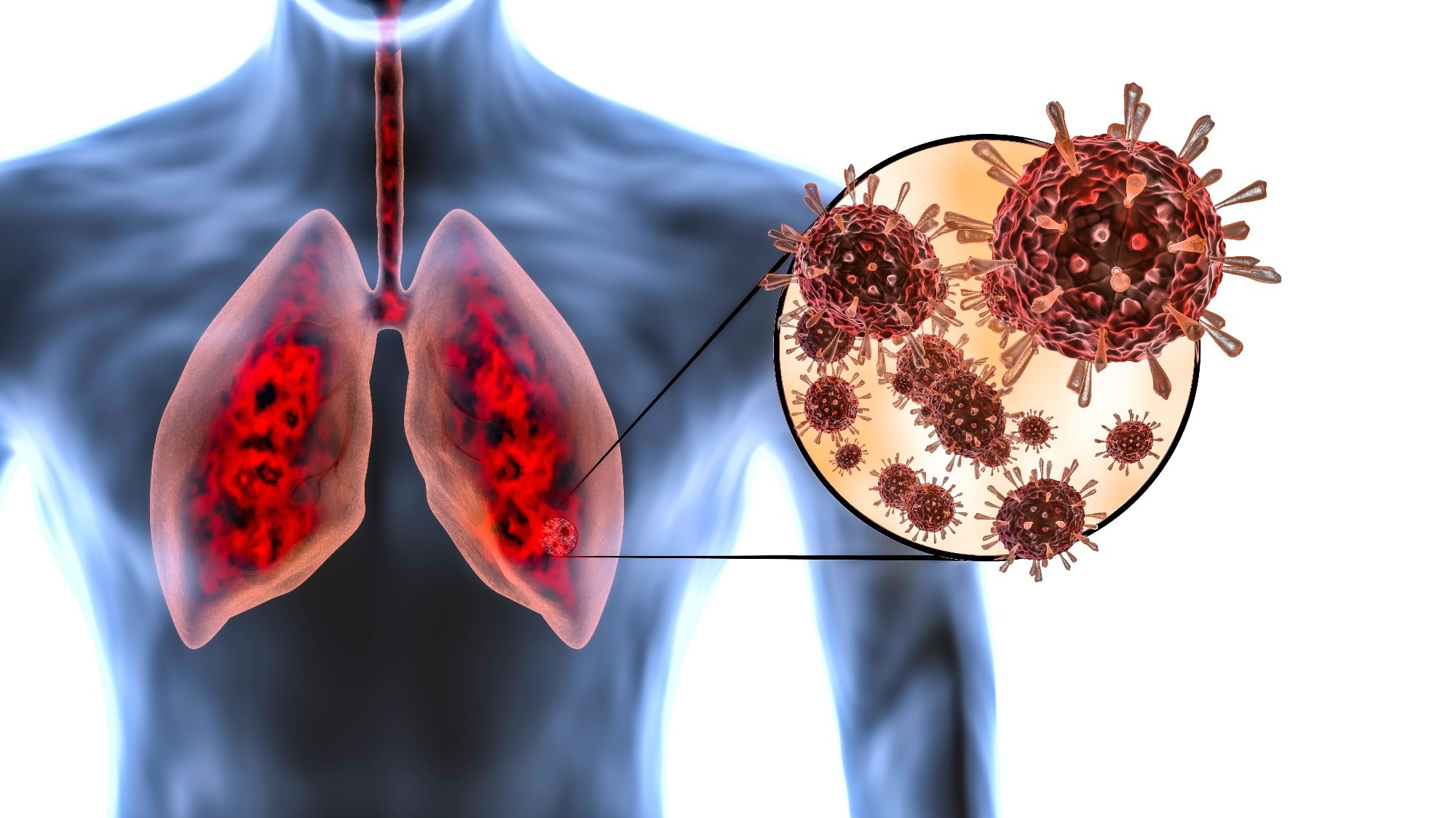
 Study: A persistent neutrophil-associated immune signature characterizes post–COVID-19 pulmonary sequelae. Image Credit: MarcinWojc / Shutterstock
Study: A persistent neutrophil-associated immune signature characterizes post–COVID-19 pulmonary sequelae. Image Credit: MarcinWojc / Shutterstock
Previous clinical studies have indicated that patients with severe COVID-19–related acute respiratory distress syndrome have a higher risk of pulmonary complications. This is because acute severe COVID-19 leads to hyperinflammation, which can be detected within the airways as well as systematically. In addition, many studies have reported myeloid cells significantly contributing to immunopathology. However, whether post–COVID-19 lung pathology is due to the persistence of such increased inflammatory response or some alternate pathways is still unknown.
Recent studies have identified an increase in CD4+T and CD8+ T lymphocytes associated with myeloid inflammation in patients with post–C OVID-19 lung parenchymal abnormalities. These studies help to understand the immunological landscape following recovery from acute COVID-19 but do not comprise an appropriate control group. Moreover, they are also unable to determine the protective and susceptible pathways associated with the development of persistent lung changes.
A new study in the journal Science Translational Medicine aimed to analyze individuals hospitalized with severe COVID-19 to compare those with persistent interstitial lung changes to those with full radiographic resolution. It also aimed to determine the immune mechanisms that lead to such downstream complications.
About the study
The study involved recruiting individuals with COVID-19 from 1st March 2020 to 1st November 2021. Information on clinical demographics was collected from all the participants. COVID-19 severity was characterized into seven categories; 1- not admitted to the hospital as well as the resumption of everyday activities, 2-not admitted to the hospital but unable to resume normal activities, 3- admitted to hospital without supplemental oxygen therapy, 4-admitted to hospital with supplemental oxygen therapy, 5-admitted to hospital with the requirement of non-invasive mechanical ventilation, high-flow nasal cannula, or both, 6-admitted to hospital with the requirement of invasive mechanical ventilation, extracorporeal membrane oxygenation, or both, and 7-death.
Participants with scores from 5 to 7 were categorized as severe, and those with 1 to 3 were mild. Nasal brushings and venous blood sampling of participants took place 3 to 6 months (visit 1) following hospital discharge, along with answering a quality-of-life questionnaire. Those with severe disease were additionally sampled six months after visit 2. Healthy participants were also recruited as controls and were sampled only once. Moreover, participants with severe disease had to undergo pulmonary function tests along with CT chest imaging. This was followed by proteomic assays, phosphoproteomic assays, and nanostring ncounter analysis. Finally, alveolar epithelial cells (AECs) were infected with the SARS-CoV-2 alpha variant, and neutrophil extracellular traps (NETs) were generated.
Study findings
The results reported that 46 individuals had severe COVID-19. Differences in plasma proteomes were observed between individuals with mild and severe disease. Sixty-three proteins were identified with altered concentrations, out of which most were upregulated, and only four were downregulated. The most increased proteins were observed to be C-X-C motif chemokine 5(CXCL5), eukaryotic translation initiation factor 4E–binding protein 1, oncostatin M, and hexamethylene bisacetamide-inducible protein. The downregulated proteins were peroxiredoxin-1(PRDX1), C-C motif chemokine ligand 11 (CCL11), tryptase alpha/beta 1 (TPSAB1), and corneodesmosin(CDSN). Moreover, enrichment of the “cytokine-mediated signaling pathway,” “immune response,” and “immune system process” have been observed 3 to 6 months following recovery from acute COVID-19.
Out of the 46 individuals, 26 were reported to have interstitial lung changes 3 to 6 months following discharge. Such changes were associated with reduced pulmonary lung function and increased symptom scores. Alteration of protein concentration was also observed in individuals with interstitial lung changes and those with full resolution. The proteins observed to be most increased were tumor necrosis factor(TNF), CCL25, CCL20, extracellular newly identified receptor for advanced glycation end-products binding protein(EN-RAGE), proinflammatory cytokines interleukin-17C (IL-17C). The downregulated proteins were observed to be similar to those observed at 3 to 6 months post-discharge. Additionally, the enrichment of “defense response,” “humoral immune response,” and “neutrophil chemotaxis.” The interstitial lung changes were also observed to be associated with a persistent plasma neutrophil-associated proinflammatory immune signature.
Furthermore, differences in nasal transcriptomes were also observed between individuals with post–COVID-19 interstitial changes compared to those with resolution. Fifty-three genes were observed to be upregulated in such individuals, mainly including neutrophilic inflammation/inflammasome or antiviral defense pathway genes. Moreover, enrichment of “cellular response to type I interferon” and “cytokine-mediated signaling pathway” were observed in these individuals.
The results also reported an increase in the total neutrophil numbers and concentration of H3R8 citrullinated nucleosomes in individuals with post–COVID-19 interstitial changes compared to those with resolution. An increase in the plasma concentration of the neutrophil protease myeloperoxidase, which is negatively correlated with lung function impairment and positively correlated with radiological disease extent, was also observed. Differences were observed between peripheral blood mononuclear cells(PBMCs) isolated from individuals with interstitial differences compared to those with resolution.
Enrichment of immunoregulatory and proliferative kinases was observed downstream of the proinflammatory cytokine receptors. Post–COVID-19 interstitial lung disease was reportedly driven by primary virus infection and host inflammatory response, with NETs being an important driving factor. Individuals with post-COVID-19 interstitial changes at visit 2 showed partial resolution of inflammatory and clinical abnormalities.
Therefore, the current study highlights the immune pathways associated with post–COVID-19 interstitial changes. The chronic inflammation that occurs in a few individuals needs further research to understand how it can be targeted.
Limitations
The study has certain limitations. First, the analysis of immune signatures took place in nasal and peripheral blood samples. Second, the study was unable to assess neutrophil subphenotypes or activation status. Third, the study is unable to remove neutrophil debris and its remnants from the PBMCs. Finally, the formation and activity of NETs are more complex in vivo and might not be recapitulated entirely in the study.