A recent study conducted by a team of Italian scientists has demonstrated that the clinical severity of coronavirus disease 2019 (COVID-19) in children depends on the dynamics of immune response induced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
The study is currently available on the Research Square* preprint server while under consideration for publication in Scientific Reports.
Background
SARS-CoV-2, the causative pathogen of COVID-19, has caused relatively less severe infection in children and adolescents throughout the pandemic. However, clinical severity has occasionally been observed in some cases, including systemic multi-inflammatory syndrome in children (MIS-C). This condition is characterized by an aberrant inflammatory response.
The reason behind the observed variation in clinical severity between children and adults is not fully known. However, it has been hypothesized that the pattern of social interactions, viral load, and age-related dynamics of immune response make children less susceptible to SARS-CoV-2 infection.
In the current study, scientists have evaluated the correlation between SARS-CoV-2-induced immune response and COVID-19 severity in children. In a subset of children with severe infection, they have characterized the dynamics of immune responses with cardiovascular manifestations.
Study population
The study involved a total of 18 hospitalized children with SARS-CoV-2 infection. The immunological profiles of infected children were compared with that of 13 healthy children (control).
The patients were categorized based on clinical severity and age. Moderate and severe infections were found in 56% and 44% of patients. The average duration of hospital stay was 12 days, with only one child admitted to the intensive care unit (ICU).
The patients with moderate infection had upper or lower respiratory tract infections without organ dysfunction. In contrast, severely infected patients experienced multiorgan failure or required oxygen supplementation. Cardiovascular involvement was evidenced in seven children.
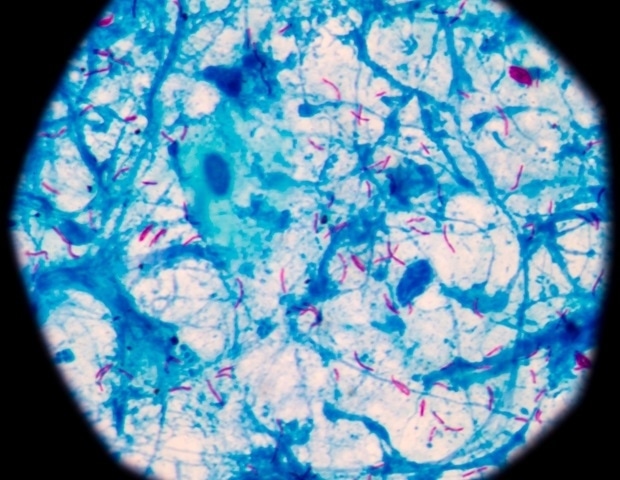
Dynamics of antibody response in SARS-CoV-2 infected children
Binding and neutralizing antibodies against SARS-CoV-2 were detected in 78% of patients.
In addition to clinical severity, age-related differences in antibody response were assessed in hospitalized children. Based on age, they were categorized as infants, children, and adolescents.
A significantly higher level of anti-spike receptor-binding domain (RBD) IgG antibodies was detected in severely infected children than in moderately infected children. A significantly higher level of anti-RBD IgM antibodies was detected in moderately infected adolescents than in severely infected infants. Regarding neutralizing antibodies, a significantly higher level was detected in severe children compared to that in severe infants.
Dynamics of inflammatory response
Patients with severe infection exhibited significantly higher levels of circulating cytokines and chemokines compared to those with moderate infection. The highest levels of cytokines and chemokines were detected in infants with severe infections.
The comparison of inflammatory and antibody responses revealed a negative correlation between antibody and cytokine/chemokine levels in infants and children with severe infection and cardiovascular involvement. In particular, anti-SARS-CoV-2 binding antibodies showed a negative correlation with interleukin 2 (IL-2).
Among infants, children, and adolescents with moderate infection, a strong correlation was observed between selected cytokines and chemokines. Considering virus-specific binding antibodies, a negative correlation was observed with IL-12 level.
In children and adolescents with moderate infection and extremely low cytokine/chemokine levels, only a weak correlation was observed between antibody and inflammatory responses. The virus-specific binding antibodies showed a negative correlation with IL-8, IL-5, and monocyte chemoattractant protein-1. Notably, circulating cytokine/chemokine profiles of these patients significantly overlapped with that of healthy children.
Significantly increased production of SARS-CoV-2-stimulated cytokines and chemokines, as well as significantly increased levels of T lymphocyte activation and migration-specific proteins were observed in SARS-CoV-2 infected children compared to that in healthy children.
Study significance
The study provides an overview of the antibody and inflammatory responses in hospitalized infants, children, and adolescents with moderate or severe SARS-CoV-2 infection. Overall, the study reveals that the dynamics of virus-induced immune response is directly correlated with disease severity and partially with age.
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.