In a recent review published in the Nutrients Journal, researchers reviewed existing data on dietary patterns, foods, and nutrients to ameliorate nonalcoholic fatty liver disease (NAFLD).
 Study: Dietary Patterns, Foods, and Nutrients to Ameliorate Non-Alcoholic Fatty Liver Disease: A Scoping Review. Image Credit: sweet marshmallow/Shutterstock.com
Study: Dietary Patterns, Foods, and Nutrients to Ameliorate Non-Alcoholic Fatty Liver Disease: A Scoping Review. Image Credit: sweet marshmallow/Shutterstock.com
Background
Despite being the most frequent cause of chronic liver disease globally, NAFLD lacks pharmaceutical therapy and dietary recommendations to address its severe health consequences.
NASH worsens cirrhosis and hepatocellular carcinoma, resulting in higher medical costs, financial losses, and a worse quality of life.
Dietary adjustments, lifestyle changes, and lifestyle modifications are examples of treatment options. Metabolic syndrome, obesity, cardiovascular disease, hypertension, diabetes, and chronic renal disease have all been associated with NAFLD.
About the review
In the present review, researchers described dietary approaches to managing NAFLD. Databases such as MEDLINE, Web of Science, Google Scholar, and Scopus were searched between January and July 2023 for relevant records published in English or Spanish.
Diets, dietary guidelines, gut microbiome, and NAFLD
The Mediterranean Diet (MedDiet) is a plant-based diet high in monounsaturated fatty acids (MUFAs) and low in red meat intake. According to research, those who eat a high-fat Western diet are more likely to acquire NAFLD and have it worsen.
The Mediterranean Diet, on the other hand, has been linked to improved hepatic steatosis and a decreased risk of NAFLD.
Low carbohydrate consumption, refined carbs, and low sugars, with olive oil providing the most added fats, distinguish MedDiet from other diets. MedDiet is linked to a decreased rate of NAFLD and a reduction in weight gain, insulin resistance, and NAFLD.
The MedDiet, due to low carbohydrate consumption and plant-rich dietary composition, offers a viable alternative to Western diets.
NAFLD, or nonalcoholic fatty liver disease, is associated with insulin resistance and a lack of phospholipid metabolism. Consumption of processed meat, red meat, soda, biscuits, and cakes has been linked to insulin resistance and NAFLD.
Saturated fats interfere with phospholipid metabolism, causing mitochondrial malfunction, increased reactive oxygen species (ROS) production, and apoptosis. High animal protein consumption has also been connected to NAFLD in obese people.
Diet directly impacts de novo lipogenesis, the process by which hepatocytes convert excess carbohydrates, particularly fructose, into fatty acids. Regular fructose consumption is linked to increased fibrosis, mostly owing to industrial fructose.
High-fructose diets comprising sucrose, fructose, and high-fructose corn syrup have been related to a heightened risk of developing steatosis and NASH, especially in overweight and obese individuals.
Genetics, foods, and NAFLD amelioration
Diet is important in developing NAFLD because it affects deoxyribonucleic acid (DNA) homeostasis and telomere biology. DNA production and repair require folate, calcium, retinol, vitamin E, and nicotinic acid, but trans fats can cause DNA damage.
Telomere shortening is detected in NAFLD, although it is prevented by fiber, omega-3-type fatty acids, and vegetables. High-glycemic index carbohydrates, processed meat, and saturated fats promote telomere shortening.
PNPLA3 (patatin-like phospholipase domain-containing 3) is a key regulator of liver fat accumulation and NAFLD development. Diets high in carbohydrates and fatty acids can lead the mutant gene to encode proteins. Diet may alter hepatic lipid utilization, insulin resistance, oxidative stress, and mitochondrial function via modulating epigenetic changes.
Betaine, choline, betaine, folate, and vitamin B12 deficiencies may promote DNA methylation, boosting hepatic triglyceride production. Consumption of nuts, seeds, seafood, and high-fiber diets considerably reduces the risk of developing NAFLD in males.
Nuts enhance lipid profiles, liver disease, and inflammation, potentially effectively treating NAFLD.
Fish can generate omega-3 fatty acids from marine plants, which can help decrease liver fat and avoid NAFLD, nonalcoholic steatohepatitis (NASH), and fibrosis.
High-fiber diets and whole grains can impact gut microbiota composition, potentially influencing the hepatic gut axis in NAFLD development. A high total legume diet (peas, lentils, and beans) is strongly associated with a decreased risk of NAFLD.
The mechanism underlying the protective benefits of vegetables and fruits on NAFLD risk is not fully understood. However, their lower energy density has been explained after addition to the diet and the antioxidant activity of polyphenols and carotenoid contents in vegetables and fruits.
Non-starchy vegetable consumption has been linked to improved metabolic outcomes, such as lower visceral and liver fat and higher insulin sensitivity.
Dairy products, particularly yogurt containing Lactobacillus acidophilus La5 and Bifidobacterium lactis Bb12, have been linked to a lower risk of NAFLD due to their high whey protein content, which helps to reduce weight and fat mass.
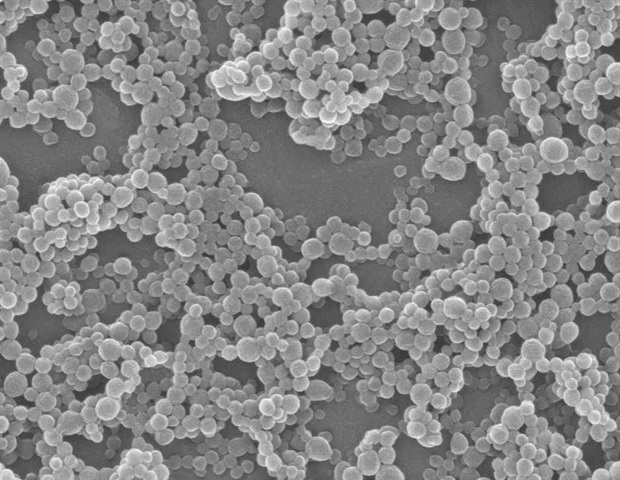
Probiotics, such as Bifidobacterium and Lactobacillus strains, have been shown to reduce oxidative and inflammatory liver damage while also decreasing hepatic triglycerides (TG) and hepatic steatosis.
Prebiotics, such as unsweetened filtered coffee, can influence the makeup of the gut microbiota, which is implicated in developing NAFLD. Choline is an important group B vitamin from food intake and endogenous production. It is mostly digested and stored in the liver.
Micronutrients implicated in NAFLD include zinc, copper, iron, selenium, magnesium, vitamins A, C, D, and E, as well as carotenoids, with antioxidant, antifibrotic, immunomodulatory, and lipoprotective properties reported as mechanisms of action.
Based on the findings, the MedDiet, which focuses on lowering oxidative stress and inflammation, can help control NAFLD.
A high-quality diet, frequent exercise, and limiting sugar consumption are important tactics, and enough fiber and coffee consumption can help guard against gut bacteria.





;Resize=(1200,627)&impolicy=perceptual&quality=mediumHigh&hash=758146986667c586a806e5c9a7b375ea92c72b851399e7c41e8a9ee2a95781d7)